

API Suppliers

US DMFs Filed
0

CEP/COS Certifications
0

JDMFs Filed
0
Other Certificates
0
Other Suppliers
0

USA (Orange Book)

Europe
0

Canada
0

Australia
0

South Africa
0
Uploaded Dossiers
0
U.S. Medicaid
Annual Reports
0
0
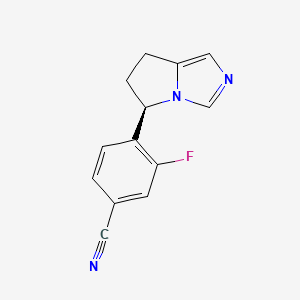
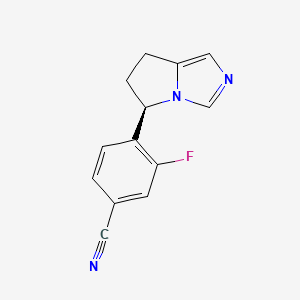
1. (+)-osilodrostat
2. 4-((5r)-6,7-dihydro-5h-pyrrolo(1,2-c)imidazol-5-yl)-3-fluoro-benzonitrile
3. Benzonitrile, 4-((5r)-6,7-dihydro-5h-pyrrolo(1,2-c)imidazol-5-yl)-3-fluoro-
4. Isturisa
5. Lci699
1. Lci699
2. 928134-65-0
3. Isturisa
4. Lci-699
5. (+)-osilodrostat
6. Lci699-nx
7. Osilodrostat Free Base
8. Lci-699-nx
9. Chembl3099695
10. 5yl4iq1078
11. (r)-4-(6,7-dihydro-5h-pyrrolo[1,2-c]imidazol-5-yl)-3-fluorobenzonitrile
12. 4-[(5r)-6,7-dihydro-5h-pyrrolo[1,2-c]imidazol-5-yl]-3-fluorobenzonitrile
13. 4-[(5r)-6,7-dihydro-5h-pyrrolo[1,2-c]imidazol-5-yl]-3-fluorobenzo Nitrile
14. 4-((5r)-6,7-dihydro-5h-pyrrolo(1,2-c)imidazol-5-yl)-3-fluoro-benzonitrile
15. 4-[(4r,5r)-6,7-dihydro-5h-pyrrolo[1,2-c]imidazol-5-yl]-3-fluorobenzonitrile
16. Benzonitrile, 4-((5r)-6,7-dihydro-5h-pyrrolo(1,2-c)imidazol-5-yl)-3-fluoro-
17. Osilodrostat [usan:inn]
18. Lci 699
19. Osilodrostat [mi]
20. Osilodrostat (usan/inn)
21. Osilodrostat [inn]
22. Osilodrostat [usan]
23. Osilodrostat [who-dd]
24. Unii-5yl4iq1078
25. Gtpl8310
26. Schembl12460772
27. Dtxsid40156570
28. Ex-a1397
29. Bdbm50444549
30. S7456
31. Zinc72318114
32. Ccg-266774
33. Cs-6896
34. Db11837
35. 1304733-26-3
36. Ac-32907
37. Bs-17881
38. Hy-16276
39. D11061
40. A909743
41. Q27088216
| Molecular Weight | 227.24 g/mol |
|---|---|
| Molecular Formula | C13H10FN3 |
| XLogP3 | 1.9 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 3 |
| Rotatable Bond Count | 1 |
| Exact Mass | 227.08587549 g/mol |
| Monoisotopic Mass | 227.08587549 g/mol |
| Topological Polar Surface Area | 41.6 Ų |
| Heavy Atom Count | 17 |
| Formal Charge | 0 |
| Complexity | 337 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 1 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Osilodrostat is indicated for the treatment of adult patients with Cushing's disease for whom pituitary surgery is not an option or has not been curative.
FDA Label
Isturisa is indicated for the treatment of endogenous Cushings syndrome in adults.
Osilodrostat lowers endogenous cortisol levels by inhibiting the enzyme that catalyzes the final step in cortisol synthesis. As endogenous cortisol levels function as a surrogate marker for drug effect, 24-hour urine free cortisol levels should be assessed 1-2x weekly during the initial titration stage and every 1-2 months thereafter to ensure cortisol levels remain physiologically appropriate. Osilodrostat is highly metabolized and requires dose adjustments in patient with hepatic dysfunction. Osilodrostat can cause a dose-dependent prolongation of the QTc interval and should be used with caution in patients with a higher baseline risk (e.g. concomitant QTc-prolonging medications, electrolyte abnormalities). Prior to beginning therapy, patients should have a baseline ECG and any electrolyte abnormalities (especially hypokalemia and/or hypomagnesemia) should be remedied. As osilodrostat halts cortisol synthesis at its final stage, its use can result in the accumulation of cortisol precursors, aldosterone precursors, and androgens. The accumulation of the cortisol precursor 11-deoxycorticosterone can activate mineralocorticoid receptors which may lead to hypokalemia, edema, or hypertension. Patients should be monitored for these symptoms as they are evidence of elevated 11-deoxycorticosterone levels, and for symptoms such as hirustism, acne, and hypertrichosis which may be suggestive of excessive circulating androgen levels.
H02CA02
H - Systemic hormonal preparations, excl. sex hormones and insulins
H02 - Corticosteroids for systemic use
H02C - Antiadrenal preparations
H02CA - Anticorticosteroids
H02CA02 - Osilodrostat
Absorption
The oral absorption of osilodrostat is rapid, with a Tmax of approximately 1 hour, and assumed to be essentially complete. Exposure (i.e. AUC and Cmax) increases slightly more than dose-proportionately over the standard dosing range. Coadministration of osilodrostat with food does not affect its pharmacokinetics to a clinically significant extent. Age and gender do not affect pharmacokinetics, but bioavailability and total exposure is higher (though not clinically significant) in patients of Asian descent. Exposure to osilodrostat is greater in patients with moderate-severe hepatic impairment - prescribing information recommends a starting dose of 1mg twice daily in patients with moderate hepatic impairment (Child-Pugh B) and a starting dose of 1mg each evening in patients with severe hepatic impairment (Child-Pugh C).
Route of Elimination
Following oral administration of radiolabeled osilodrostat, 90.6% of the radioactivity was eliminated in the urine with only 1.58% in the feces. Only 5.2% of the administered dose was eliminated in the urine as unchanged parent drug, suggesting that metabolism followed by urinary elimination is osildrostat's primary means of clearance.
Volume of Distribution
The median apparent volume of distribution of osilodrostat is 100 L.
Clearance
Data regarding the oral clearance of osilodrostat are not currently available.
Osilodrostat is extensively metabolized - approximately 80% of an orally administered dose is excreted as metabolites, and this is the predominant means of drug clearance. The most abundant metabolites in plasma are M35.4 (di-oxygenated osilodrostat), M16.5, and M24.9 at 51%, 9%, and 7% of the administered dose, respectively. The M34.5 and M24.9 metabolites have longer half-lives than the parent drug which may lead to accumulation with twice-daily dosing. Of the thirteen metabolites observed in the urine, the most abundant are M16.5 (osilodrostat glucuronide), M22 (a glucuronide conjugate of M34.5), and M24.9 at 17%, 13%, and 11% of the administered dose, respectively. The M34.5 metabolite accounts for less than 1% of the dose excreted in urine, but its glucuronide conjugate (M22) accounts for approximately 13%. The biotransformation of osilodrostat is mediated by multiple cytochrome P450 (CYP) and UDP-glucuronosyltransferase (UGT) enzymes, though no single enzyme appears to contribute >25% to the total clearance. Of the total clearance, approximately 26% is CYP-mediated, 19% is UGT-mediated, and 50% is mediated by other enzymes. The formation of M34.5, the major metabolite of osilodrostat, is likely non-CYP-mediated. The formation of osilodrostat glucuronide (M16.5), its major urinary metabolite, is catalyzed by UGT1A4, UGT2B7, and UGT2B10. _In vitro_ data suggest that none of the metabolites contribute to the therapeutic efficacy of osilodrostat, but the M34.5 metabolite has been implicated in the inhibition and/or induction of multiple enzymes and transporters.
The elimination half-life of osilodrostat is approximately 4 hours.
Cushings syndrome is an endocrine disorder resulting from chronic and excessive exposure to glucocorticoids, the symptoms of which may include thinning of the skin and hair, weight gain, muscle weakness, and osteoporosis, as well a constellation of psychiatric, cardiovascular, and immunological deficiencies. Cushings syndrome is most commonly precipitated by exogenous treatment with supraphysiological doses of glucocorticoids such as those found in nasal sprays, skin creams, and inhalers. Cushings disease - another less common cause of Cushings syndrome - is generally the result of increased endogenous cortisol exposure due to excessive secretion of adrenocroticotrophic hormone (ACTH) from a pituitary adenoma. Osilodrostat is an inhibitor of 11-hydroxylase (CYP11B1) and, to a lesser extent, aldosterone synthase (CYP11B2). The CYP11B1 enzyme is responsible for catalyzing the final step of cortisol synthesis - by inhibiting this enzyme, osilodrostat helps to normalize endogenous cortisol levels and alleviate symptoms of Cushings disease.


