1. 17 Beta Estradiol
2. 17 Beta Oestradiol
3. 17 Beta-estradiol
4. 17 Beta-oestradiol
5. Aerodiol
6. Delestrogen
7. Estrace
8. Estraderm Tts
9. Estradiol 17 Alpha
10. Estradiol 17 Beta
11. Estradiol 17beta
12. Estradiol Anhydrous
13. Estradiol Hemihydrate
14. Estradiol Hemihydrate, (17 Alpha)-isomer
15. Estradiol Monohydrate
16. Estradiol Valerate
17. Estradiol Valeriante
18. Estradiol, (+-)-isomer
19. Estradiol, (-)-isomer
20. Estradiol, (16 Alpha,17 Alpha)-isomer
21. Estradiol, (16 Alpha,17 Beta)-isomer
22. Estradiol, (17-alpha)-isomer
23. Estradiol, (8 Alpha,17 Beta)-(+-)-isomer
24. Estradiol, (8 Alpha,17 Beta)-isomer
25. Estradiol, (9 Beta,17 Alpha)-isomer
26. Estradiol, (9 Beta,17 Beta)-isomer
27. Estradiol, Monosodium Salt
28. Estradiol, Sodium Salt
29. Estradiol-17 Alpha
30. Estradiol-17 Beta
31. Estradiol-17beta
32. Oestradiol
33. Ovocyclin
34. Progynon Depot
35. Progynon-depot
36. Progynova
37. Vivelle
1. Beta-estradiol
2. 17beta-estradiol
3. 50-28-2
4. Oestradiol
5. Dihydrofolliculin
6. Estrace
7. Vivelle
8. Ovocyclin
9. Progynon
10. Dihydrotheelin
11. Dihydroxyestrin
12. Aquadiol
13. Climara
14. Diogynets
15. Divigel
16. Gynergon
17. Gynoestryl
18. Vagifem
19. Diogyn
20. Oestroglandol
21. Aerodiol
22. Corpagen
23. Dimenformon
24. Estraderm
25. Estrogel
26. Estrovite
27. Femestral
28. Follicyclin
29. Ginosedol
30. Macrodiol
31. Oestergon
32. Ovahormon
33. Ovasterol
34. Ovastevol
35. Perlatanol
36. Primofol
37. Profoliol
38. Altrad
39. Bardiol
40. Evorel
41. Femogen
42. Lamdiol
43. Syndiol
44. Dihydromenformon
45. Estradiol-17beta
46. Cis-estradiol
47. Estraderm Tts
48. Estraldine
49. Estroclim
50. Trocosone
51. Estring
52. Menorest
53. Nordicol
54. Zumenon
55. Systen
56. D-oestradiol
57. D-estradiol
58. Progynon Dh
59. Climaderm
60. Compudose
61. Dermestril
62. Estrasorb
63. Ovocycline
64. Encore
65. Innofem
66. Menest
67. Oesclim
68. Alora
69. Dihydroxyoestrin
70. 17beta-oestradiol
71. Sk-estrogens
72. Progynon-dh
73. Fempatch
74. Gynestrel
75. Gynodiol
76. Microdiol
77. Oestrogynal
78. Ovociclina
79. Ovocylin
80. Tradelia
81. Esclim
82. Estroclim 50
83. Macrol
84. Zerella
85. Oestradiol R
86. Estring Vaginal Ring
87. Dihydrofollicular Hormone
88. Trial Sat
89. Theelin, Dihydro-
90. Elestrin
91. Evamist
92. Oestrogel
93. Compudose 200
94. Compudose 365
95. Profoliol B
96. 17b-oestradiol
97. 17-beta-estradiol
98. Estradiol-17-beta
99. Estradot
100. Estrogen
101. Gelestra
102. Menostar
103. 3,17-epidihydroxyestratriene
104. Zesteem
105. Dihydroxyesterin
106. Cis-oestradiol
107. Estraderm Tts 50
108. Estrogens, Esterified
109. Nsc-9895
110. 17.beta.-estradiol
111. B-estradiol
112. Epiestriol 50
113. 17beta Oestradiol
114. 17 Beta-estradiol
115. Estradiol-17 Beta
116. Amnestrogen
117. Femanest
118. Estra-1,3,5(10)-triene-3,17beta-diol
119. 3,17-epidihydroxyoestratriene
120. Sandrena 1
121. 17b-estradiol
122. (17beta)-estra-1,3,5(10)-triene-3,17-diol
123. Estraderm (tn)
124. Estradiol Anhydrous
125. [3h]-estradiol
126. 17
127. A-estradiol
128. 17
129. A-oestradiol
130. Estrogel (tn)
131. Climara (tn)
132. Divigel (tn)
133. Estrace (tn)
134. Estring (tn)
135. Innofem (tn)
136. Vagifem (tn)
137. Vivelle (tn)
138. 17.beta.-oestradiol
139. Elestrim
140. 3,17.beta.-estradiol
141. .beta.-estradiol
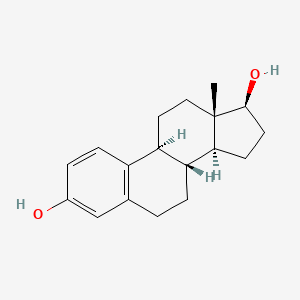
142. (8r,9s,13s,14s,17s)-13-methyl-6,7,8,9,11,12,14,15,16,17-decahydrocyclopenta[a]phenanthrene-3,17-diol
143. .beta.-oestradiol
144. [3h]]estradiol
145. Estradiol 17-beta
146. 17-beta-oestradiol
147. Estradiol, .beta.-
148. Estradiol-17.beta.
149. Chebi:16469
150. Estra-1,3,5(10)-triene-3,17-diol (17beta)-
151. Oestradiol-17.beta.
152. 17-.beta.-oestradiol
153. Estradiol Hemihydrate
154. Oestra-1,3,5(10)-triene-3,17beta-diol
155. Estrasorb (tn)
156. 17.beta.-oh-estradiol
157. 17.beta.-oh-oestradiol
158. 17beta Estradiol (e2)
159. Extrasorb
160. 17beta-estra-1,3,5(10)-triene-3,17-diol
161. Estreva
162. Estrifam
163. Femtran
164. Ginedisc
165. Nsc-20293
166. Chembl135
167. Gynpolar
168. (17beta)-estra-1(10),2,4-triene-3,17-diol
169. Sandrena Gel
170. D-3,17.beta.-estradiol
171. D-3,17.beta.-oestradiol
172. Sisare Gel
173. Estra-1,3,5(10)-triene-3,17-diol, (17beta)-
174. Estrofem 2
175. Mls000069494
176. 3,17b-dihydroxyestra-1,3,5(10)-triene
177. (+)-3,17.beta.-estradiol
178. 141290-02-0
179. Oestradiolum
180. Estradiol Valerate Metabolite E2
181. Climara Forte
182. 4ti98z838e
183. Oestradiol Berco
184. Estraderm Mx
185. Vivelle-dot
186. [3h]e2
187. Wc3011
188. Oestradiol-17beta
189. Estrapak 50
190. (1s,10r,11s,14s,15s)-15-methyltetracyclo[8.7.0.0^{2,7}.0^{11,15}]heptadeca-2(7),3,5-triene-5,14-diol
191. (8r,9s,13s,14s,17s)-13-methyl-7,8,9,11,12,13,14,15,16,17-decahydro-6h-cyclopenta[a]phenanthrene-3,17-diol
192. E2
193. Wc-3011
194. Estradiolum [inn]
195. Estradiolo [dcit]
196. Ncgc00091544-04
197. Oestradiol-17-beta
198. Estradiolum
199. Estrodiolum
200. Estradiolo
201. Femestrol
202. Smr000059126
203. Estradiol-3,17beta
204. Dsstox_cid_573
205. 17-beta-oh-estradiol
206. 3,17-beta-estradiol
207. 3,17beta-dihydroxyestra-1,3,5(10)-triene
208. 3,17-beta-oestradiol
209. D-3,17beta-estradiol
210. Estra-1,3,5(10)-triene-3,17.beta.-diol
211. 3,17.beta.-dihydroxyestra-1,3,5(10)-triene
212. E(sub 2)
213. Dsstox_rid_75666
214. Methyl 1-cyclopropyl-6,7-difluoro-8-methoxy-4-oxo-1,4-dihydroquinoline-3-carboxylate.
215. Benzogynestry
216. Dsstox_gsid_20573
217. Estropause
218. Estasorb
219. [2,4,6,7-3h]-e2
220. E 2
221. Destradiol
222. Minivelle
223. Yuvvexy
224. Zesteen
225. .alpha.-estradiol
226. 17-beta-oh-oestradiol
227. 17?-estradiol
228. D-3,17beta-oestradiol
229. D-3,17-beta-estradiol
230. Estrodiolum [inn-latin]
231. Estra-1,3,5(10)-triene-3,17-diol (17.beta.)-
232. D-3,17-beta-oestradiol
233. Activella (salt/mix)
234. Combipatch (salt/mix)
235. Ccris 280
236. Component Of Menrium
237. Estradiol-17 Alpha
238. Climara Pro (salt/mix)
239. 3,17beta-estradiol
240. 3,17-.beta.-oestradiol
241. Estraderm Tts 100
242. Hsdb 3589
243. 3,3,5(10)-triene
244. Sr-01000075866
245. 17-.beta.-estradiol
246. Einecs 200-023-8
247. 1,3,5-estratriene-3,17-beta-diol
248. Oestrodiol
249. Estradiol [usp:inn:ban]
250. 3,17beta-dihydroxyestra-1,3,5-triene
251. 3,17beta-dihydroxyoestra-1,3,5-triene
252. Delta-estradiol
253. Dihydro-theelin
254. 3,17-beta-dihydroxyoestra-1,3,5-triene
255. Unii-4ti98z838e
256. Beta -estradiol
257. Delta-oestradiol
258. Tx-004hr
259. Estra-1,3,5(10)-triene-3,17-beta-diol
260. Estradiol Complex
261. Estrogel Hbf
262. Oestra-1,3,5(10)-triene-3,17-beta-diol
263. 1jgl
264. 1lhu
265. 1qkt
266. 1qku
267. 3,17-beta-dihydroxyestra-1,3,5(10)-triene
268. [3h]estradiol
269. 1,3,5-estratriene-3,17.beta.-diol
270. 3,17-beta-dihydroxy-1,3,5(10)-oestratriene
271. Cas-50-28-2
272. 17-beta-estra-1,3,5(10)-triene-3,17-diol
273. 17beta-oestra-1,3,5(10)-triene-3,17-diol
274. .alpha.-oestradiol
275. 17-beta-oestra-1,3,5(10)-triene-3,17-diol
276. Estra-1,3,5(10)-triene-3,17-diol
277. Prestwick_207
278. 3,17b-estradiol
279. Bio-e-gel
280. Fem7
281. [3h]-estrogen
282. 17 ?-estradiol
283. 3,17.beta.-dihydroxyestra-1,3,5-triene
284. 3,17.beta.-dihydroxyoestra-1,3,5-triene
285. Cmc_11154
286. Imvexxy
287. 1,3,5,(10)-estratrien-3,17.beta.-diol
288. Sl-1100
289. Oestra-1,3,5(10)-triene-3,17.beta.-diol
290. 2j7x
291. 3,17.beta.-dihydroxy-1,3,5(10)-estratriene
292. 3,17.beta.-dihydroxy-1,3,5(10)-oestratriene
293. 3,3,5-triene
294. [3h]17beta-estradiol
295. Estradiol [inn]
296. Estradiol [jan]
297. (17?)-estra-1,3,5(10)-triene-3,17-diol
298. 17.beta.-estra-1,3,5(10)-triene-3,17-diol
299. Estradiol [mi]
300. Estradiol [hsdb]
301. Estradiol [inci]
302. 17.beta.-oestra-1,3,5(10)-triene-3,17-diol
303. Opera_id_1688
304. Prestwick0_000441
305. Prestwick1_000441
306. Prestwick2_000441
307. Prestwick3_000441
308. Spectrum5_002055
309. 17beta-estradiol (e2)
310. Estradiol [vandf]
311. 3,17beta-dihydroxy-1,3,5(10)-estratriene
312. Alpha-estradiol (obsolete)
313. Beta-estradiol, >=98%
314. Bmse000642
315. Epitope Id:136018
316. (+)-3,17b-estradiol
317. E 8875
318. Ec 200-023-8
319. Estradiol [usp-rs]
320. Estradiol [who-dd]
321. Schembl8049
322. (+)-3,17beta-estradiol
323. Estradiol (jan/usp/inn)
324. Tritiated Estradiol-17-beta
325. Bidd:pxr0065
326. Lopac0_000503
327. S-21400
328. Bspbio_000482
329. Bspbio_001065
330. Kbiogr_000405
331. Kbiogr_002269
332. Kbioss_000405
333. Kbioss_002270
334. Oestradiol-17beta And Esters
335. Mls000758312
336. Mls001076331
337. Mls001424022
338. Bidd:er0125
339. Oestradiol-17beta And Esters [steroidal Oestrogens]
340. Spbio_002421
341. Estradiol [green Book]
342. Bpbio1_000532
343. Gtpl1012
344. Gtpl1013
345. Estradiol [orange Book]
346. Dtxsid0020573
347. Niosh/kg7030000
348. Bdbm17292
349. Bijuva Component Estradiol
350. Kbio2_000405
351. Kbio2_002269
352. Kbio2_002973
353. Kbio2_004837
354. Kbio2_005541
355. Kbio2_007405
356. Kbio3_000769
357. Kbio3_000770
358. Kbio3_002749
359. Estradiol [usp Monograph]
360. Nsc9895
361. 1a52
362. 1g50
363. 2d06
364. Angeliq Component Estradiol
365. Cmap_000005
366. Estradiol Impurity A [ip]
367. Oriahnn Component Estradiol
368. Prefest Component Estradiol
369. Bio1_000403
370. Bio1_000892
371. Bio1_001381
372. Bio2_000363
373. Bio2_000843
374. Hms1362e07
375. Hms1569i04
376. Hms1792e07
377. Hms1990e07
378. Hms2051c17
379. Hms2090e18
380. Hms2096i04
381. Hms2236h04
382. Hms3261f07
383. Hms3403e07
384. Hms3713i04
385. Hms3884a08
386. Beta-estradiol, Analytical Standard
387. (8s,9s,13s,14s,17s)-13-methyl-6,7,8,9,11,12,14,15,16,17-decahydrocyclopenta[a]phenanthrene-3,17-diol
388. Activella Component Estradiol
389. Bcp08579
390. Estradiol 17-beta [vandf]
391. Hy-b0141
392. Estradiol Component Of Bijuva
393. Tox21_111148
394. Tox21_202057
395. Tox21_300288
396. Tox21_500503
397. 1,5-estratriene-3,17.beta.-diol
398. Combipatch Component Estradiol
399. Lmst02010001
400. S1709
401. Zinc13520815
402. Estradiol Component Of Angeliq
403. Estradiol Component Of Oriahnn
404. Estradiol Component Of Prefest
405. Estradiol-17-beta-6,7-(sup 3)h
406. [2,4,6,7-3h]-17beta-estradiol
407. Akos015896570
408. Climara Pro Component Estradiol
409. Ccg-100808
410. Cs-1938
411. Db00783
412. Estradiol Component Of Activella
413. Lp00503
414. Nc00058
415. Sdccgsbi-0050487.p002
416. Estradiol Component Of Combipatch
417. Idi1_002118
418. Smp1_000121
419. Ncgc00091544-00
420. Ncgc00091544-01
421. Ncgc00091544-02
422. Ncgc00091544-05
423. Ncgc00091544-06
424. Ncgc00091544-07
425. Ncgc00091544-09
426. Ncgc00091544-10
427. Ncgc00091544-11
428. Ncgc00091544-12
429. Ncgc00091544-13
430. Ncgc00091544-14
431. Ncgc00091544-15
432. Ncgc00091544-16
433. Ncgc00091544-18
434. Ncgc00091544-27
435. Ncgc00179321-01
436. Ncgc00179321-02
437. Ncgc00254177-01
438. Ncgc00259606-01
439. Ncgc00261188-01
440. 17-e
441. Ac-22346
442. As-13729
443. Cpd000059126
444. Estradiol Component Of Climara Pro
445. Estra-1,3,5(10)-triene-3,17b-diol
446. Oestra-1,3,5(10)-triene-3,17b-diol
447. Wln: L E5 B666ttt&j E1 Fq Oq
448. Estra-1,5(10)-triene-3,17.beta.-diol
449. Estradiol, Meets Usp Testing Specifications
450. 3,17beta-dihydroxyestra-1,3,5(10)-trien
451. Eu-0100503
452. Kg70300000
453. Oestra-1,5(10)-triene-3,17.beta.-diol
454. 17-beta-estradiol 100 Microg/ml In Methanol
455. 17-beta-estradiol 1000 Microg/ml In Methanol
456. C00951
457. D00105
458. (17b)-estra-1,3,5(10)-triene-3,17-diol
459. 13b-methyl-1,3,5(10)-gonatriene-3,17b-ol
460. 17-decahydrocyclopenta[a]phenanthrene-3,17-diol
461. 17.beta.-estra-1,5(10)-triene-3,17-diol
462. 17.beta.-oestra-1,5(10)-triene-3,17-diol
463. Ethinylestradiol Impurity D [ep Impurity]
464. 003e693
465. 17-beta-estradiol 100 Microg/ml In Acetonitrile
466. Q422416
467. Sr-01000721892
468. 13beta-methyl-1,3,5(10)-gonatriene-3,17beta-ol
469. Estra-1,5(10)-triene-3,17-diol (17.beta.)-
470. Estradiol Benzoate Impurity A [ep Impurity]
471. Estradiol Valerate Impurity A [ep Impurity]
472. Q-201503
473. Sr-01000075866-1
474. Sr-01000075866-4
475. Sr-01000721892-3
476. Brd-k18910433-001-04-4
477. Brd-k18910433-001-43-2
478. Estra-1(10),2,4-triene-3,17-diol, (17beta)-
479. Estra-1,5(10)-triene-3,17-diol, (17.beta.)-
480. Z1847670481
481. B8b5aef5-4957-49eb-a14f-444a8212c482
482. Beta-estradiol, Bioreagent, Powder, Suitable For Cell Culture
483. Estradiol, United States Pharmacopeia (usp) Reference Standard
484. 13.beta.-methyl-1,3,5(10)-gonatriene-3,17.beta.-ol
485. Beta-estradiol, Powder, Gamma-irradiated, Suitable For Cell Culture
486. Estra-1,3,5(10)-triene-3,17-diol, (6,7-(sup 3)h,17-beta)-
487. (9beta,13alpha,14beta,17alpha)-estra-1,3,5(10)-triene-3,17-diol
488. Estradiol, Pharmaceutical Secondary Standard; Certified Reference Material
489. (13s,17s)-13-methyl-7,8,9,11,12,13,14,15,16,17-decahydro-6h-cyclopenta[a]phenanthrene-3,17-beta-diol
490. (1s,10r,11s,14s,15s)-15-methyltetracyclo[8.7.0.0;{2,7}.0;{11,15}]heptadeca-2,4,6-triene-5,14-diol
491. 17beta-estradiol Solution, 1.0 Mg/ml In Acetonitrile, Ampule Of 1 Ml, Certified Reference Material
| Molecular Weight | 272.4 g/mol |
|---|---|
| Molecular Formula | C18H24O2 |
| XLogP3 | 4 |
| Hydrogen Bond Donor Count | 2 |
| Hydrogen Bond Acceptor Count | 2 |
| Rotatable Bond Count | 0 |
| Exact Mass | 272.177630004 g/mol |
| Monoisotopic Mass | 272.177630004 g/mol |
| Topological Polar Surface Area | 40.5 Ų |
| Heavy Atom Count | 20 |
| Formal Charge | 0 |
| Complexity | 382 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 5 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Estradiol tablets are indicated in the treatment of moderate to severe vasomotor symptoms associated with the menopause. /Included in US product label/
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
Estradiol tablets are indicated in the treatment of moderate to severe symptoms of vulvar and vaginal atrophy associated with the menopause. When prescribing solely for the treatment of symptoms of vulvar and vaginal atrophy, topical vaginal products should be considered. /Included in US product label/
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
Estradiol tablets are indicated in the treatment of hypoestrogenism due to hypogonadism, castration or primary ovarian failure. /Included in US product label/
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
Estradiol tablets are indicated in the treatment of breast cancer (for palliation only) in appropriately selected women and men with metastatic disease. /Included in US product label/
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
For more Therapeutic Uses (Complete) data for ESTRADIOL (7 total), please visit the HSDB record page.
ESTROGENS INCREASE THE RISK OF ENDOMETRIAL CANCER- Close clinical surveillance of all women taking estrogens is important. Adequate diagnostic measures, including endometrial sampling when indicated, should be undertaken to rule out malignancy in all cases of undiagnosed persistent or recurring abnormal vaginal bleeding. There is no evidence that the use of "natural" estrogens results in a different endometrial risk profile than "synthetic" estrogens at equivalent estrogen doses.
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
CARDIOVASCULAR AND OTHER RISKS- Estrogens with or without progestins should not be used for the prevention of cardiovascular disease.
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
The Women's Health Initiative (WHI) study reported increased risks of myocardial infarction, stroke, invasive breast cancer, pulmonary emboli, and deep vein thrombosis in postmenopausal women (50 to 79 years of age) during 5 years of treatment with oral conjugated estrogens (CE 0.625 mg) combined with medroxyprogesterone acetate (MPA 2.5 mg) relative to placebo.
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
The Women's Health Initiative Memory Study (WHIMS), a substudy of WHI, reported increased risk of developing probable dementia in postmenopausal women 65 years of age or older during 4 years of treatment with oral conjugated estrogens plus medroxyprogesterone acetate relative to placebo. It is unknown whether this finding applies to younger postmenopausal women or to women taking estrogen alone therapy.
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
For more Drug Warnings (Complete) data for ESTRADIOL (48 total), please visit the HSDB record page.
Estradiol is indicated in various preparations for the treatment of moderate to severe vasomotor symptoms and vulvar and vaginal atrophy due to menopause, for the treatment of hypoestrogenism due to hypogonadism, castration, or primary ovarian failure, and for the prevention of postmenopausal osteoporosis. It is also used for the treatment of breast cancer (only for palliation therapy) in certain men or women with metastatic disease, and for the treatment of androgen-dependent prostate cancer (only for palliation therapy). It is also used in combination with other hormones as a component of oral contraceptive pills for preventing pregnancy (most commonly as [DB00977], a synthetic form of estradiol). **A note on duration of treatment** Recommendations for treatment of menopausal symptoms changed drastically following the release of results and early termination of the Women's Health Initiative (WHI) studies in 2002 as concerns were raised regarding estrogen use. Specifically, the combined estrogenprogestin group was discontinued after about 5 years of follow up due to a statistically significant increase in invasive breast cancer and in cardiovascular events. Following extensive critique of the WHI results, Hormone Replacement Therapy (HRT) is now recommended to be used only for a short period (for 3-5 years postmenopause) in low doses, and in women without a history of breast cancer or increased risk of cardiovascular or thromboembolic disease. Estrogen for postmenopausal symptoms should always be given with a progestin component due to estrogen's stimulatory effects on the endometrium; in women with an intact uterus, unopposed estrogen has been shown to promote the growth of the endometrium which can lead to endometrial hyperplasia and possibly cancer over the long-term.
FDA Label
Estradiol acts on the on the estrogen receptors to relieve vasomotor systems (such as hot flashes) and urogenital symptoms (such as vaginal dryness and dyspareunia). Estradiol has also been shown to exert favorable effects on bone density by inhibiting bone resorption. Estrogen appears to inhibit bone resorption and may have beneficial effects on the plasma lipid profile. Estrogens cause an increase in hepatic synthesis of various proteins, which include sex hormone binding globulin (SHBG), and thyroid-binding globulin (TBG). Estrogens are known to suppress the formation of follicle-stimulating hormone (FSH) in the anterior pituitary gland. **A note on hyper-coagulable state, cardiovascular health, and blood pressure** Estradiol may cause an increased risk of cardiovascular disease, DVT, and stroke, and its use should be avoided in patients at high risk of these conditions. Estrogen induces a hyper-coagulable state, which is also associated with both estrogen-containing oral contraceptive (OC) use and pregnancy. Although estrogen causes an increase in levels of plasma renin and angiotensin. Estrogen-induced increases in angiotensin, causing sodium retention, which is likely to be the mechanism causing hypertension after oral contraceptive treatment.
Estrogens
Compounds that interact with ESTROGEN RECEPTORS in target tissues to bring about the effects similar to those of ESTRADIOL. Estrogens stimulate the female reproductive organs, and the development of secondary female SEX CHARACTERISTICS. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. (See all compounds classified as Estrogens.)
G - Genito urinary system and sex hormones
G03 - Sex hormones and modulators of the genital system
G03C - Estrogens
G03CA - Natural and semisynthetic estrogens, plain
G03CA03 - Estradiol
Absorption
The absorption of several formulations of estradiol is described below: Oral tablets and injections First-pass metabolism in the gastrointestinal tract rapidly breaks down estradiol tablets before entering the systemic circulation. The bioavailability of oral estrogens is said to be 2-10% due to significant first-pass effects. The esterification of estradiol improves the administration (such as with estradiol valerate) or to sustain release from intramuscular depot injections (including estradiol cypionate) via higher lipophilicity. After absorption, the esters are cleaved, which leads to the release of endogenous estradiol, or 17-estradiol. Transdermal preparations The transdermal preparations slowly release estradiol through intact skin, which sustains circulating levels of estradiol during a 1 week period of time. Notably, the bioavailability of estradiol after transdermal administration is about 20 times higher than after oral administration. Transdermal estradiol avoids first pass metabolism effects that reduce bioavailability. Administration via the buttock leads to a Cmax of about 174 pg/mL compared to 147 pg/mL via the abdomen. Spray preparations After daily administration, the spray formulations of estradiol reach steady state within 7-8 days. After 3 sprays daily, Cmax is about 54 pg/mL with a Tmax of 20 hours. AUC is about 471 pghr/mL. Vaginal ring and cream preparations Estradiol is efficiently absorbed through the mucous membranes of the vagina. The vaginal administration of estrogens evades first-pass metabolism. Tmax after vaginal ring delivery ranges from 0.5 to 1 hour. Cmax is about 63 pg/mL. The vaginal cream preparation has a Cmax of estradiol (a component of Premarin vaginal estrogen conjugate cream) was a Cmax of 12.8 16.6 pg/mL, Tmax of 8.5 6.2 hours, with an AUC of 231 285 pghr/mL.
Route of Elimination
Estradiol is excreted in the urine with both glucuronide and sulfate conjugates.
Volume of Distribution
Estrogens administered exogenously distribute in a similar fashion to endogenous estrogens. They can be found throughout the body, especially in the sex hormone target organs, such as the breast, ovaries and uterus.
Clearance
In one pharmacokinetic study, the clearance of orally administered micronized estradiol in postmenopausal women was 29.915.5 mL/min/kg. Another study revealed a clearance of intravenously administered estradiol was 1.3 mL/min/kg.
Estrogens used in therapeutics are well absorbed through the skin, mucous membranes, and the gastrointestinal (GI) tract. The vaginal delivery of estrogens circumvents first-pass metabolism.
US Natl Inst Health; DailyMed. Current Medication Information ESTRING (estradiol) ring (October 2009). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=11686
The Estradiol Transdermal System Continuous Delivery (Once-Weekly) continuously releases estradiol which is transported across intact skin leading to sustained circulating levels of estradiol during a 7 day treatment period. The systemic availability of estradiol after transdermal administration is about 20 times higher than that after oral administration. This difference is due to the absence of first-pass metabolism when estradiol is given by the transdermal route.
US Natl Inst Health; DailyMed. Current Medication Information ESTRADIOL patch (September 2009). Available from, as of February 23, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=12806
In a Phase I study of 14 postmenopausal women, the insertion of ESTRING (estradiol vaginal ring) rapidly increased serum estradiol (E2) levels. The time to attain peak serum estradiol levels (Tmax) was 0.5 to 1 hour. Peak serum estradiol concentrations post-initial burst declined rapidly over the next 24 hours and were virtually indistinguishable from the baseline mean (range: 5 to 22 pg/mL). Serum levels of estradiol and estrone (E1) over the following 12 weeks during which the ring was maintained in the vaginal vault remained relatively unchanged
Table: PHARMACOKINETIC MEAN ESTIMATES FOLLOWING SINGLE ESTRING APPLICATION [Table#4651]
US Natl Inst Health; DailyMed. Current Medication Information ESTRING (estradiol) ring (October 2009). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=11686
[Table#4651]
The initial estradiol peak post-application of the second ring in the same women resulted in ~38 percent lower Cmax, apparently due to reduced systemic absorption via the treated vaginal epithelium. The relative systemic exposure from the initial peak of ESTRING accounted for approximately 4 percent of the total estradiol exposure over the 12-week period.
US Natl Inst Health; DailyMed. Current Medication Information ESTRING (estradiol) ring (October 2009). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=11686
For more Absorption, Distribution and Excretion (Complete) data for ESTRADIOL (17 total), please visit the HSDB record page.
Exogenously administered estrogens are metabolized in the same fashion as endogenous estrogens. Metabolic transformation occurs primarily in the liver and intestine. Estradiol is metabolized to estrone, and both are converted to estriol, which is later excreted in the urine. Sulfate and glucuronide conjugation estrogens also take place in the liver. Biliary secretion of metabolic conjugates are released into the intestine, and estrogen hydrolysis in the gut occurs, followed by reabsorption. The CYP3A4 hepatic cytochrome enzyme is heavily involved in the metabolism of estradiol. CYP1A2 also plays a role.
Exogenous estrogens are metabolized in the same manner as endogenous estrogens. Circulating estrogens exist in a dynamic equilibrium of metabolic interconversions. These transformations take place mainly in the liver. Estradiol is converted reversibly to estrone, and both can be converted to estriol, which is the major urinary metabolite. Estrogens also undergo enterohepatic recirculation via sulfate and glucuronide conjugation in the liver, biliary secretion of conjugates into the intestine, and hydrolysis in the gut followed by reabsorption. In postmenopausal women, a significant proportion of the circulating estrogens exist as sulfate conjugates, especially estrone sulfate, which serves as a circulating reservoir for the formation of more active estrogens.
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006).
Variations in estradiol metabolism ... depend upon the stage of the menstrual cycle ... In general, the hormone undergoes rapid hepatic biotransformation with a plasma half-life measured in minutes.
Hardman, J.G., L.E. Limbird, P.B. Molinoff, R.W. Ruddon, A.G. Goodman (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics. 9th ed. New York, NY: McGraw-Hill, 1996., p. 1420
Estradiol is primarily converted ... to estriol, which is the major urinary metabolite. A variety of sulfate and glucuronide conjugates also are excreted in the urine.
Hardman, J.G., L.E. Limbird, P.B. Molinoff, R.W. Ruddon, A.G. Goodman (eds.). Goodman and Gilman's The Pharmacological Basis of Therapeutics. 9th ed. New York, NY: McGraw-Hill, 1996., p. 1420
The metabolism of estradiol-17beta and estrone is similar in rats and in humans, in that both species transform these steroids mainly by (aromatic) 2-hydroxylation, and also by 16alpha-hydroxylation. Glucuronides of the various metabolites are excreted in the bile. Differences in the metabolism of estrogens by humans and rats lie mostly in the type of conjugation. A relatively large proportion of administered estrone, estradiol-17beta and estriol is transformed in rats to metabolites oxygenated both at C-2 and C-16. When estriol is administered to rats, glucuronides and, to a lesser extent, sulfates of 16-ketooestradiol and of 2- and 3-methyl ethers of 2-hydroxyoestriol and 2-hydroxy-16-ketooestradiol are excreted in the bile. In contrast, hydroxylations at C-6 or C-7 of ring B of estradiol-17beta and estrone are a minor pathway in rats. 2-Hydroxyoestrogens ('catechol estrogens') are further transformed by various routes, including covalent binding to proteins.
IARC. Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. Geneva: World Health Organization, International Agency for Research on Cancer, 1972-PRESENT. (Multivolume work). Available at: https://monographs.iarc.fr/ENG/Classification/index.php, p. V21 307 (1979)
For more Metabolism/Metabolites (Complete) data for ESTRADIOL (8 total), please visit the HSDB record page.
The terminal half-lives for various estrogen products post oral or intravenous administration has been reported to range from 1-12 hours. One pharmacokinetic study of oral estradiol valerate administration in postmenopausal women revealed a terminal elimination half-life of 16.9 6.0 h. A pharmacokinetic study of intravenous estradiol administration in postmenopausal women showed an elimination half-life of 27.45 5.65 minutes. The half-life of estradiol appears to vary by route of administration.
... After oral administration ... the terminal half life was 20.1 hr ...
IARC. Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. Geneva: World Health Organization, International Agency for Research on Cancer, 1972-PRESENT. (Multivolume work). Available at: https://monographs.iarc.fr/ENG/Classification/index.php, p. V72 476 (1999)
Estrogen is found in the the breast, uterine, ovarian, skin, prostate, bone, fat, and brain tissues. The main source of estrogen in adult women during the reproductive period of life is the ovarian follicle, which secretes 70 to 500 mcg of estradiol each day. After menopause, however, the majority of endogenous estrogen is produced by transformation of androstenedione (which is secreted by the adrenal cortex) to estrone in the peripheral tissues. Both estrone and its sulphate conjugated form, estrone sulphate, represent the most abundant estrogens found in postmenopausal women. Estradiol, however, is considerably more potent than estrone and estriol at the estrogen receptor (ER). As a result, the higher estrone concentration in postmenopausal population, can cause various undesirable effects. These effects may include hot flashes, chills, vaginal dryness, mood swings, irregular menstruation, and chills, in addition to sleep problems. Estradiol workings by binding to subtypes of the estrogen receptor: estrogen receptor alpha (ER) and estrogen receptor beta (ER). It also exerts potent agonism of G Protein-coupled estrogen receptor (GPER), which is recognized an important regulator of this drug's rapid effects. Once the estrogen receptor has bound to its ligand, it enters the nucleus of the target cell, regulating gene transcription and formation of of messenger RNA. This mRNA makes contact with ribosomes producing specific proteins that express the effect of estradiol upon the target cell. Agonism of estrogen receptors increases pro-estrogenic effects, leading to the relief of vasomotor and urogenital symptoms of a postmenopausal or low estradiol state.
Endogenous estrogens are largely responsible for the development and maintenance of the female reproductive system and secondary sexual characteristics. Although circulating estrogens exist in a dynamic equilibrium of metabolic interconversions, estradiol is the principal intracellular human estrogen and is substantially more potent than its metabolites, estrone and estriol at the receptor level. ... After menopause, most endogenous estrogen is produced by conversion of androstenedione, secreted by the adrenal cortex, to estrone by peripheral tissues. Thus, estrone and the sulfate conjugated form, estrone sulfate, are the most abundant circulating estrogens in postmenopausal women. Estrogens act through binding to nuclear receptors in estrogen-responsive tissues. To date, two estrogen receptors have been identified. These vary in proportion from tissue to tissue. Circulating estrogens modulate the pituitary secretion of the gonadotropins, luteinizing hormone (LH) and follicle stimulating hormone (FSH), through a negative feedback mechanism. Estrogens act to reduce the elevated levels of these hormones seen in postmenopausal women.
US Natl Inst Health; DailyMed. Current Medication Information estrace (estradiol) tablet (August 2006). Available from, as of February 22, 2010: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?id=1485
Estrogens have an important role in the reproductive, skeletal, cardiovascular, and central nervous systems in women, and act principally by regulating gene expression. Biologic response is initiated when estrogen binds to a ligand-binding domain of the estrogen receptor resulting in a conformational change that leads to gene transcription through specific estrogen response elements (ERE) of target gene promoters; subsequent activation or repression of the target gene is mediated through 2 distinct transactivation domains (ie, AF-1 and AF-2) of the receptor. The estrogen receptor also mediates gene transcription using different response elements (ie, AP-1) and other signal pathways. Recent advances in the molecular pharmacology of estrogen and estrogen receptors have resulted in the development of selective estrogen receptor modulators (eg, clomiphene, raloxifene, tamoxifen, toremifene), agents that bind and activate the estrogen receptor but that exhibit tissue-specific effects distinct from estrogen. Tissue-specific estrogen-agonist or -antagonist activity of these drugs appears to be related to structural differences in their estrogen receptor complex (eg, specifically the surface topography of AF-2 for raloxifene) compared with the estrogen (estradiol)-estrogen receptor complex. A second estrogen receptor also has been identified, and existence of at least 2 estrogen receptors (ER-alpha, ER-beta) may contribute to the tissue-specific activity of selective modulators. While the role of the estrogen receptor in bone, cardiovascular tissue, and the CNS continues to be studied, emerging evidence indicates that the mechanism of action of estrogen receptors in these tissues differs from the manner in which estrogen receptors function in reproductive tissue. /Estrogen General Statement/
American Society of Health System Pharmacists; AHFS Drug Information 2010. Bethesda, MD. (2010), p. 3130
Intracellular cytosol-binding proteins for estrogens have been identified in estrogen-responsive tissues including the female genital organs, breasts, pituitary, and hypothalamus. The estrogen-binding protein complex (ie, cytosol-binding protein and estrogen) distributes into the cell nucleus where it stimulates DNA, RNA, and protein synthesis. The presence of these receptor proteins is responsible for the palliative response to estrogen therapy in women with metastatic carcinoma of the breast. /Estrogen General Statement/
American Society of Health System Pharmacists; AHFS Drug Information 2010. Bethesda, MD. (2010), p. 3130
Estrogens have generally favorable effects on blood cholesterol and phospholipid concentrations. Estrogens reduce LDL-cholesterol and increase HDL-cholesterol concentrations in a dose-related manner. The decrease in LDL-cholesterol concentrations associated with estrogen therapy appears to result from increased LDL catabolism, while the increase in triglyceride concentrations is caused by increased production of large, triglyceride-rich, very-low-density lipoproteins (VLDLs); changes in serum HDL-cholesterol concentrations appear to result principally from an increase in the cholesterol and apolipoprotein A-1 content of HDL2- and a slight increase in HDL3-cholesterol. /Estrogen General Statement/
American Society of Health System Pharmacists; AHFS Drug Information 2010. Bethesda, MD. (2010), p. 3130
For more Mechanism of Action (Complete) data for ESTRADIOL (7 total), please visit the HSDB record page.
MARKET PLACE

Reply
20 Jun 2022
Reply
21 Feb 2019
 FULL SCREEN VIEW Click here to open all results in a new tab [this preview display 10 results]
FULL SCREEN VIEW Click here to open all results in a new tab [this preview display 10 results]

