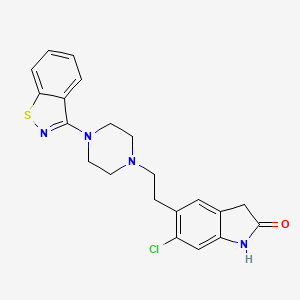
1. 5-(2-(4-(3-benzisothiazolyl)piperazinyl)ethyl)-6-chloro-1,3-dihydro-2h-indol-2-one
2. Cp 88059
3. Cp 88059-01
4. Cp-88,059
5. Cp-88,059-01
6. Cp-88,059-1
7. Geodon
8. Ziprasidone Hydrochloride
9. Ziprasidone Hydrochloride, Monohydrate
10. Ziprazidone
1. 146939-27-7
2. Geodon
3. Zeldox
4. Zipradon
5. Ziprasidone (inn)
6. Cp 88059
7. 5-[2-[4-(1,2-benzothiazol-3-yl)piperazin-1-yl]ethyl]-6-chloro-1,3-dihydroindol-2-one
8. 6uka5vej6x
9. Chembl708
10. 5-(2-(4-(benzo[d]isothiazol-3-yl)piperazin-1-yl)ethyl)-6-chloroindolin-2-one
11. Cp-88059
12. Chebi:10119
13. Ziprasidone [inn]
14. Dsstox_cid_3753
15. Ziprasidone [inn:ban]
16. 5-{2-[4-(1,2-benzothiazol-3-yl)piperazin-1-yl]ethyl}-6-chloro-2,3-dihydro-1h-indol-2-one
17. Dsstox_rid_77186
18. Dsstox_gsid_23753
19. 2h-indol-2-one, 5-[2-[4-(1,2-benzisothiazol-3-yl)-1-piperazinyl]ethyl]-6-chloro-1,3-dihydro-
20. Ziprasidona
21. Ziprasidonum
22. Zipradon (tn)
23. 2h-indol-2-one, 5-(2-(4-(1,2-benzisothiazol-3-yl)-1-piperazinyl)ethyl)-6-chloro-1,3-dihydro-
24. 5-(2-(4-(1,2-benzisothiazol-3-yl)-1-piperazinyl)ethyl)-6-chloro-1,3-dihydro-2h-indol-2-one
25. 5-[2-[4-(1,2-benzisothiazol-3-yl)-1-piperazinyl]ethyl]-6-chloro-1,3-dihydro-2h-indol-2-one
26. Cas-146939-27-7
27. Ncgc00186050-01
28. Unii-6uka5vej6x
29. Cp-88059-27
30. Hsdb 7745
31. Ziprasidone-[d8]
32. Ziprasidone- Bio-x
33. Ziprasidone [mi]
34. Ziprasidone [hsdb]
35. Gtpl59
36. C07568
37. Ziprasidone [vandf]
38. 5-{2-[4-(1,2-benzothiazol-3-yl)piperazin-1-yl]ethyl}-6-chloro-1,3-dihydro-2h-indol-2-one
39. Ziprasidone [mart.]
40. Schembl28028
41. Ziprasidone [who-dd]
42. Mls000759435
43. Bidd:gt0042
44. Dtxsid4023753
45. Hms3742m19
46. Zinc538550
47. Bvb74558
48. Tox21_112194
49. Tox21_113525
50. Bdbm50048803
51. Akos015900383
52. Tox21_112194_1
53. Am90310
54. Cs-1071
55. Db00246
56. Sdccgsbi-0633778.p001
57. 5-{2-[4-(1,2-benzisothiazol-3-yl)piperazin-1-yl]ethyl}-6-chloro-1,3-dihydro-2h-indol-2-one
58. Ncgc00263539-01
59. Ncgc00263539-03
60. Ncgc00263539-05
61. Ncgc00263539-13
62. Ac-23360
63. Bz164575
64. Hy-14542
65. Smr000466328
66. Ft-0654208
67. Ft-0655916
68. Z0034
69. Vu0286234-2
70. D08687
71. D92803
72. Ab00639925-02
73. Ab00639925-04
74. Ab00639925_05
75. Ab00639925_06
76. 883z936
77. A807468
78. A808568
79. L000659
80. Q205517
81. Cp 88059;cp-88059;cp88059
82. 5-[2-(4-benzo[d]isothiazol-3-yl-piperazin-1-yl)-ethyl]-6-chloro-1,3-dihydro-indol-2-one
83. Cp88059;5-[2-[4-(1,2-benzothiazol-3-yl)piperazin-1-yl]ethyl]-6-chloro-indolin-2-one
84. 5-(2-(4-(1,2-benzisothiazol-3-yl)-1-piperazinyl)-ethyl)-6-chloro-1,3-dihydro-2h-indol-2-one
85. 5-(2-(4-(1,2-benzisothiazol-3-yl)-1-piperazinyl)ethyl)-6-chloro-1,3-dihydro-2h-indole-2-one
86. 5-[2-(4-benzo[d]isothiazol-3-yl-piperazin-1-yl)-ethyl]-6-chloro-1,3-dihydro-indol-2-one (ziprasidone)
87. 5-[2-(4-benzo[d]isothiazol-3-yl-piperazin-1-yl)-ethyl]-6-chloro-1,3-dihydro-indol-2-one(norastemizole)
88. 5-[2-[4-(1,2-benzisothiazol-3-yl)-1-piperazinyl]ethyl]-6-chloro-1,3-dihydro-2h-indol-2-one Hydrochloride Monohydrate
89. Ziprasidone Solution, 1.0 Mg/ml In 1,2-dimethoxyethane, Ampule Of 1 Ml, Certified Reference Material
| Molecular Weight | 412.9 g/mol |
|---|---|
| Molecular Formula | C21H21ClN4OS |
| XLogP3 | 4 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 5 |
| Rotatable Bond Count | 4 |
| Exact Mass | 412.1124602 g/mol |
| Monoisotopic Mass | 412.1124602 g/mol |
| Topological Polar Surface Area | 76.7 Ų |
| Heavy Atom Count | 28 |
| Formal Charge | 0 |
| Complexity | 573 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 3 | |
|---|---|
| Drug Name | GEODON |
| Active Ingredient | ZIPRASIDONE MESYLATE |
| Company | PFIZER (Application Number: N020919) |
| 2 of 3 | |
|---|---|
| Drug Name | GEODON |
| Active Ingredient | ZIPRASIDONE HYDROCHLORIDE |
| Company | PFIZER (Application Number: N020825. Patents: 6150366, 6245766) |
| 3 of 3 | |
|---|---|
| Drug Name | ZIPRASIDONE HYDROCHLORIDE |
| Active Ingredient | ZIPRASIDONE HYDROCHLORIDE |
| Company | APOTEX INC (Application Number: A077561); AUROBINDO PHARMA LTD (Application Number: A204117); DR REDDYS LABS INC (Application Number: A077565); LUPIN PHARMS (Application Number: A077560); MACLEODS PHARMS LTD (Application Number: A204375); MYLAN PHARMS INC (Application Number: A202395); SANDOZ INC (Application Number: A077562); WOCKHARDT LTD (Application Number: A090348); ZYDUS PHARMS USA INC (Application Number: A208988) |
Antipsychotic Agents; Dopamine Antagonists; Serotonin Antagonists
National Library of Medicine's Medical Subject Headings. Ziprasidone. Online file (MeSH, 2015). Available from, as of Septmeber 2, 2015: https://www.nlm.nih.gov/mesh/MBrowser.html
Ziprasidone is indicated for the treatment of schizophrenia. The efficacy of oral ziprasidone was established in four short-term (4- and 6-week) controlled trials of adult schizophrenic inpatients and in one maintenance trial of stable adult schizophrenic inpatients. /Included in US product label/
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of March 30, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
Ziprasidone is indicated as monotherapy for the acute treatment of manic or mixed episodes associated with bipolar I disorder. Efficacy was established in two 3-week monotherapy studies in adult patients /Included in US product label/
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of March 30, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
Ziprasidone is indicated as an adjunct to lithium or valproate for the maintenance treatment of bipolar I disorder. Efficacy was established in a maintenance trial in adult patients. The efficacy of ziprasidone as monotherapy for the maintenance treatment of bipolar I disorder has not been systematically evaluated in controlled clinical trials /Included in US product label/
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of March 30, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
/BOXED WARNING/ WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS. Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Analyses of seventeen placebo-controlled trials (modal duration of 10 weeks), largely in patients taking atypical antipsychotic drugs, revealed a risk of death in drug-treated patients of between 1.6 to 1.7 times the risk of death in placebo-treated patients. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5%, compared to a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. Observational studies suggest that, similar to atypical antipsychotic drugs, treatment with conventional antipsychotic drugs may increase mortality. The extent to which the findings of increased mortality in observational studies may be attributed to the antipsychotic drug as opposed to some characteristic(s) of the patients is not clear. Ziprasidone is not approved for the treatment of patients with Dementia-Related Psychosis.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of March 30, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
Contraindications /include/ known history of QT prolongation (including congenital long QT syndrome), recent acute myocardial infarction, or uncompensated heart failure. Concomitant therapy with other drugs that prolong the QT interval. Known hypersensitivity to ziprasidone.
American Society of Health-System Pharmacists 2015; Drug Information 2015. Bethesda, MD. 2015, p. 2496
Geriatric patients with dementia-related psychosis treated with atypical antipsychotic drugs appear to be at an increased risk of death compared with that among patients receiving placebo. Analyses of seventeen placebo-controlled trials (average duration of 10 weeks) revealed an approximate 1.6 - to 1.7-fold increase in mortality among geriatric patients receiving atypical antipsychotic drugs (ie, aripiprazole, olanzapine, quetiapine, risperidone) compared with that in patients receiving placebo. Over the course of a typical 10-week controlled trial, the rate of death in drug-treated patients was about 4.5% compared with a rate of about 2.6% in the placebo group. Although the causes of death were varied, most of the deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature. The manufacturer states that ziprasidone is not approved for the treatment of patients with dementia-related psychosis.
American Society of Health-System Pharmacists 2015; Drug Information 2015. Bethesda, MD. 2015, p. 2496
Prolongation of the QT interval can result in an occurrence of ventricular arrhythmias (eg, torsades de pointes) and/or sudden death. In one study, oral ziprasidone prolonged the QT interval on ECG by a mean of 9-14 msec more than that observed in patients receiving risperidone, olanzapine, quetiapine, or haloperidol, but approximately 14 msec less than that observed in patients receiving thioridazine. ... Patients at particular risk of torsades de pointes and/or sudden death include those with bradycardia, hypokalemia, or hypomagnesemia, those receiving concomitant therapy with other drugs that prolong the QTC interval, and those with congenital prolongation of QTC interval. The manufacturer states that ziprasidone should be avoided in patients with congenital prolongation of the QT interval or a history of cardiac arrhythmias and in those receiving concomitant therapy with other drugs that prolong the QTC interval.
American Society of Health-System Pharmacists 2015; Drug Information 2015. Bethesda, MD. 2015, p. 2496
For more Drug Warnings (Complete) data for Ziprasidone (28 total), please visit the HSDB record page.
In its oral form, ziprasidone is approved for the treatment of schizophrenia, as monotherapy for acute treatment of manic or mixed episodes related to bipolar I disorder, and as adjunctive therapy to lithium or valproate for maintenance treatment of bipolar I disorder. The injectable formulation is approved only for treatment of acute agitation in schizophrenia.
Ziprasidone is classified as a "second generation" or "atypical" antipsychotic and is a dopamine and 5HT2A receptor antagonist with a unique receptor binding profile. As previously mentioned, ziprasidone has a very high 5-HT2A/D2 affinity ratio, binds to multiple serotonin receptors in addition to 5-HT2A, and blocks monoamine transporters which prevents 5HT and NE reuptake. On the other hand, ziprasidone has a low affinity for muscarinic cholinergic M1, histamine H1, and alpha1-adrenergic receptors.
Dopamine Antagonists
Drugs that bind to but do not activate DOPAMINE RECEPTORS, thereby blocking the actions of dopamine or exogenous agonists. Many drugs used in the treatment of psychotic disorders (ANTIPSYCHOTIC AGENTS) are dopamine antagonists, although their therapeutic effects may be due to long-term adjustments of the brain rather than to the acute effects of blocking dopamine receptors. Dopamine antagonists have been used for several other clinical purposes including as ANTIEMETICS, in the treatment of Tourette syndrome, and for hiccup. Dopamine receptor blockade is associated with NEUROLEPTIC MALIGNANT SYNDROME. (See all compounds classified as Dopamine Antagonists.)
Antipsychotic Agents
Agents that control agitated psychotic behavior, alleviate acute psychotic states, reduce psychotic symptoms, and exert a quieting effect. They are used in SCHIZOPHRENIA; senile dementia; transient psychosis following surgery; or MYOCARDIAL INFARCTION; etc. These drugs are often referred to as neuroleptics alluding to the tendency to produce neurological side effects, but not all antipsychotics are likely to produce such effects. Many of these drugs may also be effective against nausea, emesis, and pruritus. (See all compounds classified as Antipsychotic Agents.)
Serotonin Antagonists
Drugs that bind to but do not activate serotonin receptors, thereby blocking the actions of serotonin or SEROTONIN RECEPTOR AGONISTS. (See all compounds classified as Serotonin Antagonists.)
N - Nervous system
N05 - Psycholeptics
N05A - Antipsychotics
N05AE - Indole derivatives
N05AE04 - Ziprasidone
Absorption
In the absence of food, ziprasidone's oral bioavailability is 60%, and absorption may reach 100% if ziprasidone is taken with a meal containing at least 500 kcal. The difference in bioavailability has little to do with the fat content of the food and appears to be related to the bulk of the meal since more absorption occurs the longer ziprasidone remains in the stomach.
Route of Elimination
Ziprasidone is extensively metabolized after oral administration with only a small amount excreted in the urine (<1%) or feces (<4%) as unchanged drug.
Volume of Distribution
The mean apparent volume of distribution of Ziprasidone is 1.5 L/kg.
Clearance
The mean apparent systemic clearance is 7.5 mL/min/kg.
Ziprasidone is well absorbed after oral administration, reaching peak plasma concentrations in 6 to 8 hours. The absolute bioavailability of a 20 mg dose under fed conditions is approximately 60%. The absorption of ziprasidone is increased up to two-fold in the presence of food.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
The bioavailability of ziprasidone administered intramuscularly is 100%. After intramuscular administration of single doses, peak serum concentrations typically occur at approximately 60 minutes post-dose or earlier ...
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
Steady-state concentrations are achieved within one to three days of dosing. The mean apparent systemic clearance is 7.5 mL/min/kg.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
Ziprasidone has a mean apparent volume of distribution of 1.5 L/kg. It is greater than 99% bound to plasma proteins, binding primarily to albumin and alpha1-acid glycoprotein.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
For more Absorption, Distribution and Excretion (Complete) data for Ziprasidone (11 total), please visit the HSDB record page.
Ziprasidone is heavily metabolized in the liver with less than 5% of the drug excreted unchanged in the urine. The primary reductive pathway is catalyzed by aldehyde oxidase, while 2 other less prominent oxidative pathways are catalyzed by CYP3A4. Ziprasidone is unlikely to interact with other medications metabolized by CYP3A4 since only 1/3 of the antipsychotic is metabolized by the CYP3A4 system. There are 12 identified ziprasidone metabolites (abbreviations italicized): Ziprasidone sulfoxide, ziprasidone sulfone, (6-chloro-2-oxo-2,3-dihydro-1H-indol-5-yl)acetic acid (_OX-COOH_), OX-COOH glucuronide, 3-(piperazine-1-yl)-1,2-benzisothiazole (_BITP_), BITP sulfoxide, BITP sulfone, BITP sulfone lactam, S-Methyl-dihydro-ziprasidone, S-Methyl-dihydro-ziprasidone-sulfoxide, 6-chloro-5-(2-piperazin-1-yl-ethyl)-1,3-dihydro-indol-2-one (_OX-P_), and dihydro-ziprasidone-sulfone. As suggested by the quantity of metabolites, ziprasidone is metabolized through several different pathways. Ziprasidone is sequentially oxidized to ziprasidone sulfoxide and ziprasidone sulfone, and oxidative N-dealkylation of ziprasidone produces OX-COOH and BITP. OX-COOH undergoes phase II metabolism to yield a glucuronidated metabolite while BITP is sequentially oxidized into BITP sulfoxide, BITP sulfone, then BITP sulfone lactam. Ziprasidone can also undergo reductive cleavage and methylation to produce S-Methyl-dihydro-ziprasidone and then further oxidation to produce S-Methyl-dihydro-ziprasidone-sulfoxide. Finally dearylation of ziprasidone produces OX-P, and the process of hydration and oxidation transforms the parent drug into dihydro-ziprasidone-sulfone. Although CYP3A4 and aldehyde oxidase are the primary enzymes involved in ziprasidone metabolism, the pathways associated with each enzyme have not been specified.
Ziprasidone is extensively metabolized in the liver principally via reduction by aldehyde oxidase with minimal excretion of unchanged drug in urine or feces. About one-third of ziprasidone's metabolic clearance is mediated by the cytochrome P-450 (CYP) 3A4 isoenzyme.
American Society of Health-System Pharmacists 2015; Drug Information 2015. Bethesda, MD. 2015, p. 2496
Ziprasidone is primarily cleared via three metabolic routes to yield four major circulating metabolites, benzisothiazole (BITP) sulphoxide, BITP-sulphone, ziprasidone sulphoxide, and S-methyl-dihydroziprasidone.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
In vitro studies using human liver subcellular fractions indicate that S-methyl-dihydroziprasidone is generated in two steps. The data indicate that the reduction reaction is mediated by aldehyde oxidase and the subsequent methylation is mediated by thiol methyltransferase.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
In vitro studies using human liver microsomes and recombinant enzymes indicate that CYP3A4 is the major CYP contributing to the oxidative metabolism of ziprasidone. CYP1A2 may contribute to a much lesser extent. Based on in vivo abundance of excretory metabolites, less than one-third of ziprasidone metabolic clearance is mediated by cytochrome P450 catalyzed oxidation and approximately two-thirds via reduction by aldehyde oxidase. There are no known clinically relevant inhibitors or inducers of aldehyde oxidase.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
The metabolism and excretion of ziprasidone (5-[2-[4-(1,2-benzisothiazol-3-yl)piperazin-1-yl]ethyl]-6-+++chloroindolin-2-one hydrochloride hydrate) were studied in Long Evans rats after oral administration of a single dose of a mixture of 14C- and 3H-labeled ziprasidone. ... Ziprasidone was extensively metabolized in rats, and only a small amount of ziprasidone was excreted as unchanged drug. Twelve metabolites were identified ... The structures of eight metabolites were unambiguously confirmed by coelution on HPLC with synthetic standards, and four additional metabolites were partially identified. There was a gender-related difference in the excretion of urinary metabolites in Long Evans rats. The major route of metabolism in male rats involved N-dealkylation. In female rats the major metabolites were due to oxidation at the benzisothiazole ring. Based on the structures of these metabolites, four major and two minor routes of metabolism of ziprasidone were identified. The major routes included 1) N-dealkylation of the ethyl side chain attached to the piperazinyl nitrogen, 2) oxidation at the sulfur, resulting in the formation of sulfoxide and sulfone, 3) oxidation on the benzisothiazole moiety (other than sulfur), and 4) hydration of the C==N bond and subsequent oxidation at the sulfur of the benzisothiazole moiety. The minor routes involved N-oxidation on the piperazine ring and hydrolysis of the oxindole moiety.
PMID:9029052 Prakash C et al; Drug Metab Dispos 25 (2): 206-18 (1997)
Ziprasidone has known human metabolites that include 3-(1-Piperazinyl)-1,2-benzisothiazole, 6-Chloro-5-ethyl-1,3-dihydroindol-2-one, and Ziprasidone Sulfoxide.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
The half life of ziprasidone is 6-7 hours.
Elimination of ziprasidone is mainly via hepatic metabolism with a mean terminal half-life of about 7 hours within the proposed clinical dose range.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
The mean t(1/2), z in the young men, young women, elderly men and elderly women were 3.1, 4.1, 5.7 and 5.3 hr, respectively.
PMID:10771449 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2015054 Wilner KD et al; Br J Clin Pharmacol 49 (Suppl 1): 15S-20S (2000)
The effects of ziprasidone are differentiated from other antispychotics based on its preference and affinity for certain receptors. Ziprasidone binds to serotonin-2A (5-HT2A) and dopamine D2 receptors in a similar fashion to other atypical antipsychotics; however, one key difference is that ziprasidone has a higher 5-HT2A/D2 receptor affinity ratio when compared to other antipsychotics such as olanzapine, quetiapine, risperidone, and aripiprazole. Ziprasidone offers enhanced modulation of mood, notable negative symptom relief, overall cognitive improvement and reduced motor dysfunction which is linked to it's potent interaction with 5-HT2C, 5-HT1D, and 5-HT1A receptors in brain tissue. Ziprasidone can bind moderately to norepinephrine and serotonin reuptake sites which may contribute to its antidepressant and anxiolytic activity. Patient's taking ziprasidone will likely experience a lower incidence of orthostatic hypotension, cognitive disturbance, sedation, weight gain, and disruption in prolactin levels since ziprasidone has a lower affinity for histamine H1, muscarinic M1, and alpha1-adrenoceptors.
Ziprasidone is a benzisothiazolyl piperazine-derivative antipsychotic agent that is chemically unrelated to other currently available antipsychotic agents (eg, butyrophenones, phenothiazines) and has been referred to as an atypical or second-generation antipsychotic agent. The exact mechanism of antipsychotic action of ziprasidone has not been fully elucidated but, like that of other atypical antipsychotic agents (eg, olanzapine, risperidone), may involve antagonism of central type 2 serotonergic (5-HT2) receptors and central dopamine D2 receptors. As with other drugs that are effective in bipolar disorder, the precise mechanism of antimanic action of ziprasidone has not been fully elucidated. Antagonism of various other receptors (eg, histamine H1 receptors, alpha1-adrenergic receptors) may contribute to other therapeutic and adverse effects (eg, orthostatic hypotension, somnolence) observed with ziprasidone.
American Society of Health System Pharmacists; AHFS Drug Information 2009. Bethesda, MD. (2009), p. 2507
Ziprasidone exhibited high in vitro binding affinity for the dopamine D2 and D3, the serotonin 5HT2A, 5HT2C, 5HT1A, 5HT1D, and alpha1-adrenergic receptors (Ki s of 4.8, 7.2, 0.4, 1.3, 3.4, 2, and 10 nM, respectively), and moderate affinity for the histamine H1 receptor (Ki=47 nM). Ziprasidone functioned as an antagonist at the D2, 5HT2A, and 5HT1D receptors, and as an agonist at the 5HT1A receptor. Ziprasidone inhibited synaptic reuptake of serotonin and norepinephrine. No appreciable affinity was exhibited for other receptor/binding sites tested, including the cholinergic muscarinic receptor (IC50 >1 uM).
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
Antagonism at receptors other than dopamine and 5HT2 with similar receptor affinities may explain some of the other therapeutic and side effects of ziprasidone. Ziprasidone's antagonism of histamine H1 receptors may explain the somnolence observed with this drug. Ziprasidone's antagonism of alpha1-adrenergic receptors may explain the orthostatic hypotension observed with this drug.
NIH; DailyMed. Current Medication Information for Ziprasidone- ziprasidone hydrochloride capsule (Revised: December 2014). Available from, as of September 2, 2015: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=315e24c2-2f8c-47d9-b1b1-ce006646098a
c-Fos immunohistochemistry was performed on paraformaldehyde-fixed cryosections of rat brains obtained, initially, from animals 2, 4, or 6 hr after oral administration of 10 mg/kg ziprasidone or vehicle and, subsequently, from animals 2 hr after oral administration of 1, 3, or 10 mg/kg ziprasidone or vehicle. The density of immunoreactive nuclei was assessed in pre-determined forebrain regions. Ziprasidone induced a time-dependent increase in the density of c-Fos-positive nuclei that was maximal at 2 hr. At the 2 hr time-point, c-Fos expression was significantly (p<0.05) elevated in the shell and core of the nucleus accumbens, lateral and medial caudate putamen, and lateral septum. At 4 hr post-dose, c-Fos expression was also significantly increased in the cingulate gyrus. Ziprasidone-induced c-Fos expression was dose-dependent with significant (p<0.05) c-Fos expression observed in the nucleus accumbens (shell and core) and caudate putamen (lateral and medial) at 3 and 10 mg/kg and in the lateral septum at 10 mg/kg. Increased c-Fos expression in the nucleus accumbens and lateral septum is considered to be predictive of activity against positive symptoms, in the caudate putamen of motor side effect liability, and in the cingulate gyrus of efficacy against negative symptoms. Thus, the observed pattern of c-Fos expression induced in rat brain by ziprasidone is consistent with its reported clinical effects...
PMID:16328378 Jennings CA et al; Psychopharmacology (Berl) 184 (1): 13-20 (2006)
... The mechanism of action for antipsychotics has not been fully elucidated, but the hypothermia induced by this class of medications is believed to be driven through the antagonism of the dopamine (D(1-4)) and 5-hydroxytryptamine-2 (5-HT2) receptors. It has been theorized that under normal conditions, there is a balance between dopamine acting to reduce the body temperature and 5-HT2 acting to elevate body temperature. Atypical antipsychotics, particularly ziprasidone, appear to have a higher affinity to antagonize the 5-HT2 receptor and less at the D(2) receptor, therefore creating an imbalance favoring the lowering of core body temperature. Other theories include the antagonism of alpha(1) receptors by these medications causing vasodilatation and shunting of blood to the skin causing profound heat loss. ...
PMID:18606348 Gibbons GM et al; Am J Emerg Med 26 (6): 737.e1-2 (2008)

