1. Brulamycin
2. Nebcin
3. Nebicin
4. Nebramycin Factor 6
5. Obracin
6. Sulfate, Tobramycin
7. Tobracin
8. Tobramycin Sulfate
1. 32986-56-4
2. Nebramycin Factor 6
3. Nebramycin Vi
4. Nebramycin 6
5. Tobi
6. 3'-deoxykanamycin B
7. Tobramicin
8. Tobrex
9. Aktob
10. Nebcin
11. Deoxykanamycin B
12. Tobramycin Base
13. Tobi Podhaler
14. Vantobra
15. Tobradistin
16. Bethkis
17. Kitabis Pak
18. Tobramycin Sulfate
19. Nebramycin
20. Distobram
21. Tobralex
22. Tobracin (tn)
23. Nsc 180514
24. Tobrex (tn)
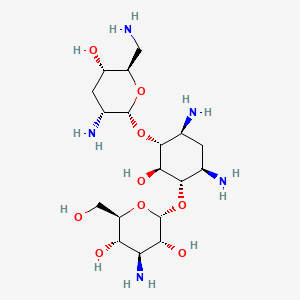
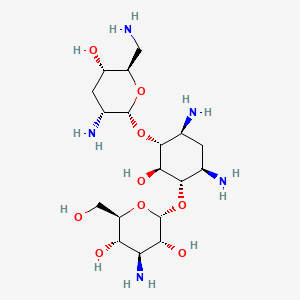
25. C18h37n5o9
26. Vz8rrz51vk
27. (2s,3r,4s,5s,6r)-4-amino-2-[(1s,2s,3r,4s,6r)-4,6-diamino-3-[(2r,3r,5s,6r)-3-amino-6-(aminomethyl)-5-hydroxyoxan-2-yl]oxy-2-hydroxycyclohexyl]oxy-6-(hydroxymethyl)oxane-3,5-diol
28. Obramycin
29. Chebi:28864
30. 1-epitobramycin
31. Nsc-180514
32. Tobramicina
33. Tobramycine
34. Tobramycinum
35. Gotabiotic
36. Nebicin
37. Tobacin
38. Tobrased
39. (1s,2s,3r,4s,6r)-4,6-diamino-3-[(2,6-diamino-2,3,6-trideoxy-alpha-d-ribo-hexopyranosyl)oxy]-2-hydroxycyclohexyl 3-amino-3-deoxy-alpha-d-glucopyranoside
40. (2s,3r,4s,5s,6r)-4-amino-2-(((1s,2s,3r,4s,6r)-4,6-diamino-3-(((2r,3r,5s,6r)-3-amino-6-(aminomethyl)-5-hydroxytetrahydro-2h-pyran-2-yl)oxy)-2-hydroxycyclohexyl)oxy)-6-(hydroxymethyl)tetrahydro-2h-pyran-3,5-diol
41. Tobramycine [inn-french]
42. Tobramycinum [inn-latin]
43. Tobramicina [inn-spanish]
44. O-3-amino-3-deoxy-?-d-glucopyranosyl-(1-6)-o-[2,6-diamino-2,3,6-trideoxy-?-d-ribohexopyranosyl-(1-4)]-2-deoxy-d-streptamine
45. O-3-amino-3-deoxy-alpha-d-glucopyranosyl-(1-4)-o-(2,6-diamino-2,3,6-trideoxy-alpha-d-ribohexopyranosyl-(1-4))-2-deoxy-d-streptamine
46. Toy
47. Nebramycin Factir 6
48. Hsdb 3259
49. Sr-05000001726
50. Einecs 251-322-5
51. Unii-vz8rrz51vk
52. Sprc-ab01
53. Brn 1357507
54. Torbamycin
55. Kitabis
56. Tobramycin Solution For Inhalation
57. Tobramycin,(s)
58. Nebcin (sulfate)
59. Ncgc00016814-01
60. (2s,3r,4s,5s,6r)-4-amino-2-((1s,2s,3r,4s,6r)-4,6-diamino-3-((2r,3r,5s,6r)-3-amino-6-(aminomethyl)-5-hydroxytetrahydro-2h-pyran-2-yloxy)-2-hydroxycyclohexyloxy)-6-(hydroxymethyl)tetrahydro-2h-pyran-3,5-diol
61. D-streptamine, O-3-amino-3-deoxy-.alpha.-d-glucopyranosyl-(1->6)-o-(2,6-diamino-2,3,6-trideoxy-.alpha.-d-ribo-hexopyranosyl-(1->4))-2-deoxy-
62. D-streptamine, O-3-amino-3-deoxy-.alpha.-d-glucopyranosyl-(1->6)-o-[2,6-diamino-2,3,6-trideoxy-.alpha.-d-ribo-hexopyranosyl-(1->4)]-2-deoxy-
63. Bethkis (tn)
64. Cas-32986-56-4
65. Tobramycin Deuterated
66. D-streptamine, O-3-amino-3-deoxy-alpha-d-glucopyranosyl-(1-6)-o-(2,6-diamino-2,3,6-trideoxy-alpha-d-ribo-hexopyranosyl-(1-4))-2-deoxy-
67. Tobramycin [2m+h]
68. Tobramycin [usan:usp:inn:ban:jan]
69. Tobi (tn)
70. Spectrum_001072
71. Tobramycin [mi]
72. Tobramycin [inn]
73. Tobramycin [jan]
74. Prestwick3_000544
75. Spectrum2_000078
76. Spectrum3_000588
77. Spectrum4_000752
78. Spectrum5_001038
79. Tobramycin [hsdb]
80. Tobramycin [usan]
81. Dsstox_cid_3680
82. Tobramycin [vandf]
83. Tobramycin (jp17/usp)
84. Schembl2838
85. Tobramycin [mart.]
86. Chembl1747
87. Dsstox_rid_77144
88. Tobramycin [usp-rs]
89. Tobramycin [who-dd]
90. Dsstox_gsid_23680
91. Bspbio_000587
92. Bspbio_002036
93. Kbiogr_001104
94. Kbioss_001552
95. 4-(2,6-diamino-2,3,6-trideoxy-alpha-d-glycopyranosyl)-6-(3-amino-3-deoxy-alpha-d-glycopyranosyl)-2-deoxystreptamine
96. Mls000069544
97. O-3-amino-3-deoxy-alpha-d-glucopyranosyl-(1-6)-o-(2,6-diamino-2,3,6-trideoxy-alpha-d-ribohexopyranosyl-(1-4))-2-deoxy-d-streptamine
98. Streptamine, O-3-amino-3-deoxy-alpha-d-glucopyranosyl-(1-4)-o-(2,6-diamino-2,3,6-tyrideoxy-alpha-d-ribohexopyranosyl-(1-6))-2-deoxy-, D-
99. Bidd:gt0503
100. Spectrum1500579
101. Spbio_000295
102. Bpbio1_000647
103. Dtxsid8023680
104. Tobramycin [orange Book]
105. Gtpl10930
106. Kbio2_001552
107. Kbio2_004120
108. Kbio2_006688
109. Kbio3_001536
110. Zylet Component Tobramycin
111. Tobramycin [ep Monograph]
112. Hms2090b16
113. Hms2092m17
114. Hms2096n09
115. Hms3713n09
116. Pharmakon1600-01500579
117. Tobramycin [usp Monograph]
118. Hy-b0441
119. Tobradex Component Tobramycin
120. Zinc8214692
121. Tobramycin 100 Microg/ml In Water
122. Tobramycin Component Of Zylet
123. Tox21_110626
124. Bdbm50366778
125. Ccg-39936
126. Nsc757352
127. S2514
128. Tobrasone Component Tobramycin
129. Tobradex (tobramycin + Dexamethasone)
130. Akos016339662
131. Db00684
132. Ks-1405
133. Nsc-757352
134. Tobradex St Component Tobramycin
135. Tobramycin Component Of Tobradex
136. Tobramycin Component Of Tobrasone
137. Ncgc00178852-01
138. Ncgc00178852-02
139. (2s,3r,4s,5s,6r)-4-amino-2-[(1s,2s,3r,4s,6r)-4,6-diamino-3-[(2r,3r,5s,6r)-3-amino-6-(aminomethyl)-5-hydroxy-tetrahydropyran-2-yl]oxy-2-hydroxy-cyclohexoxy]-6-(hydroxymethyl)tetrahydropyran-3,5-diol
140. 4-amino-2-[4,6-diamino-3-(3-amino-6-aminomethyl-5-hydroxy-tetrahydro-pyran-2-yloxy)-2-hydroxy-cyclohexyloxy]-6-hydroxymethyl-tetrahydro-pyran-3,5-diol
141. O-3-amino-3-deoxy-alpha-d-glucopyranosyl-(1-4)-o-(2,6-diamino-2,3,6-trideoxy-alpha-d-ribo-hexopyranosyl-(1-6))-2-deoxy-l-streptamine
142. Smr000058793
143. Streptamine, O-3-amino-3-deoxy-alpha-d-glucopyranosyl-(1-4)-o-(2,6-diamino-2,3,6-trideoxy-alpha-d-ribohexopyranosyl-(1-6))-2-deoxy-, D-
144. Sbi-0051915.p003
145. Tobramycin Component Of Tobradex St
146. Ab00513858
147. T2503
148. C00397
149. D00063
150. Ab00052438-12
151. Ab00052438_13
152. Ab00052438_14
153. 986t564
154. Sr-01000721898
155. Tobramycin, Antibiotic For Culture Media Use Only
156. Q-201837
157. Q1758380
158. Sr-01000721898-2
159. Sr-05000001726-1
160. Sr-05000001726-2
161. Brd-k05619559-001-12-7
162. (1s,2s,3r,4s,6r)-4,6-diamino-3-(2,6-diamino-2,3,6-trideoxy-alpha-d-ribo-hexopyranosyloxy)-2-hydroxycyclohexyl 3-amino-3-deoxy-alpha-d-glucopyranoside
163. (2s,3r,4s,5s,6r)-4-amino-2-{[(1s,2s,3r,4s,6r)-4,6-diamino-3-{[(2r,3r,5s,6r)-3-amino-6-(aminomethyl)-5-hydroxyoxan-2-yl]oxy}-2-hydroxycyclohexyl]oxy}-6-(hydroxymethyl)oxane-3,5-diol
164. D-streptamine, O-3-amino-3-deoxy-.alpha.-d-glucopyranosyl-(1->6)-o-[2,6-diamino-2,3,6-trideoxy-.alpha.-d-ribohexopyranosyl-(1->4)]-2-deoxy-
165. D-streptamine, O-3-amino-3-deoxy-.alpha.-d-glucopyranosyl-(1?6)-o-[2,6-diamino-2,3,6-trideoxy-.alpha.-d-ribo-hexopyranosyl-(1?4)]-2-deoxy-
166. O-[3-amino-3-deoxy-alpha-d-glucopyranosyl-(1->6)]-o-[2,6-diamino-2,3,6-trideoxy-alpha-d-ribo-hexopyranosyl-(1->4)]-2-deoxy-d-streptamine
167. O-3-amino-3-deoxy-.alpha.-d-glucopyranosyl-(1->4)-o-(2,6-diamino-2,3,6-trideoxy-.alpha.-d-ribo-hexopyranosyl-(1.alpha.6))-2-deoxy-l-streptamine
| Molecular Weight | 467.5 g/mol |
|---|---|
| Molecular Formula | C18H37N5O9 |
| XLogP3 | -6.2 |
| Hydrogen Bond Donor Count | 10 |
| Hydrogen Bond Acceptor Count | 14 |
| Rotatable Bond Count | 6 |
| Exact Mass | 467.25912777 g/mol |
| Monoisotopic Mass | 467.25912777 g/mol |
| Topological Polar Surface Area | 268 Ų |
| Heavy Atom Count | 32 |
| Formal Charge | 0 |
| Complexity | 609 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 14 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 12 | |
|---|---|
| Drug Name | Aktob |
| Drug Label | TOBREX (tobramycin ophthalmic ointment) 0.3% is a sterile topical ophthalmic antibiotic formulation prepared specifically for topical therapy of external ophthalmic infections.Each gram of TOBREX (tobramycin ophthalmic ointment) 0.3% contains: Acti... |
| Active Ingredient | Tobramycin |
| Dosage Form | Solution/drops |
| Route | Ophthalmic |
| Strength | 0.3% |
| Market Status | Prescription |
| Company | Akorn |
| 2 of 12 | |
|---|---|
| Drug Name | Tobi |
| PubMed Health | Tobramycin (By breathing) |
| Drug Classes | Antibiotic |
| Drug Label | TOBIis a tobramycin solution for inhalation. It is a sterile, clear, slightly yellow, non-pyrogenic, aqueous solution with the pH and salinity adjusted specifically for administration by a compressed air driven reusable nebulizer. The chemical fo... |
| Active Ingredient | Tobramycin |
| Dosage Form | Solution |
| Route | Inhalation |
| Strength | 300mg/5ml |
| Market Status | Prescription |
| Company | Novartis Pharms |
| 3 of 12 | |
|---|---|
| Drug Name | Tobradex |
| PubMed Health | Tobramycin |
| Drug Classes | Antibiotic |
| Active Ingredient | Dexamethasone; tobramycin |
| Dosage Form | Ointment; Suspension/drops |
| Route | Ophthalmic |
| Strength | 0.1%; 0.3% |
| Market Status | Prescription |
| Company | Alcon |
| 4 of 12 | |
|---|---|
| Drug Name | Tobramycin |
| PubMed Health | Tobramycin |
| Drug Classes | Antibiotic |
| Drug Label | Tobramycin sulfate, a water-soluble antibiotic of the aminoglycoside group, is derived from the actinomycete Streptomyces tenebrarius. Tobramycin Injection USP is a clear and colorless sterile aqueous solution for parenteral administration.Tobramycin... |
| Active Ingredient | Tobramycin |
| Dosage Form | Solution/drops; Solution |
| Route | Ophthalmic; Inhalation, nebulizer; Inhalation |
| Strength | 300mg/5ml; 0.3% |
| Market Status | Tentative Approval; Prescription |
| Company | Teva Pharms Usa; Pulmoflow; Bausch And Lomb; Fera Pharms; Akorn |
| 5 of 12 | |
|---|---|
| Drug Name | Tobramycin sulfate |
| PubMed Health | Tobramycin and Dexamethasone (Ophthalmic route) |
| Drug Classes | Adrenal Glucocorticoid, Aminoglycoside, Aminoglycoside/Corticosteroid Combination |
| Drug Label | Tobramycin sulfate, a water-soluble antibiotic of the aminoglycoside group, is derived from the actinomycete Streptomyces tenebrarius. Tobramycin Injection USP is a clear and colorless sterile aqueous solution for parenteral administration.Tobramycin... |
| Active Ingredient | Tobramycin sulfate |
| Dosage Form | Injectable |
| Route | Injection |
| Strength | eq 40mg base/ml; eq 10mg base/ml; eq 1.2gm base/vial |
| Market Status | Prescription |
| Company | Hospira; X Gen Pharms; Teva Pharms Usa; Xellia Pharms Aps; Fresenius Kabi Usa; Hikma Maple; Agila Speclts; Akorn |
| 6 of 12 | |
|---|---|
| Drug Name | Tobrex |
| Active Ingredient | Tobramycin |
| Dosage Form | Solution/drops; Ointment |
| Route | Ophthalmic |
| Strength | 0.3% |
| Market Status | Prescription |
| Company | Alcon; Falcon Pharms |
| 7 of 12 | |
|---|---|
| Drug Name | Aktob |
| Drug Label | TOBREX (tobramycin ophthalmic ointment) 0.3% is a sterile topical ophthalmic antibiotic formulation prepared specifically for topical therapy of external ophthalmic infections.Each gram of TOBREX (tobramycin ophthalmic ointment) 0.3% contains: Acti... |
| Active Ingredient | Tobramycin |
| Dosage Form | Solution/drops |
| Route | Ophthalmic |
| Strength | 0.3% |
| Market Status | Prescription |
| Company | Akorn |
| 8 of 12 | |
|---|---|
| Drug Name | Tobi |
| PubMed Health | Tobramycin (By breathing) |
| Drug Classes | Antibiotic |
| Drug Label | TOBIis a tobramycin solution for inhalation. It is a sterile, clear, slightly yellow, non-pyrogenic, aqueous solution with the pH and salinity adjusted specifically for administration by a compressed air driven reusable nebulizer. The chemical fo... |
| Active Ingredient | Tobramycin |
| Dosage Form | Solution |
| Route | Inhalation |
| Strength | 300mg/5ml |
| Market Status | Prescription |
| Company | Novartis Pharms |
| 9 of 12 | |
|---|---|
| Drug Name | Tobradex |
| PubMed Health | Tobramycin |
| Drug Classes | Antibiotic |
| Active Ingredient | Dexamethasone; tobramycin |
| Dosage Form | Ointment; Suspension/drops |
| Route | Ophthalmic |
| Strength | 0.1%; 0.3% |
| Market Status | Prescription |
| Company | Alcon |
| 10 of 12 | |
|---|---|
| Drug Name | Tobramycin |
| PubMed Health | Tobramycin |
| Drug Classes | Antibiotic |
| Drug Label | Tobramycin sulfate, a water-soluble antibiotic of the aminoglycoside group, is derived from the actinomycete Streptomyces tenebrarius. Tobramycin Injection USP is a clear and colorless sterile aqueous solution for parenteral administration.Tobramycin... |
| Active Ingredient | Tobramycin |
| Dosage Form | Solution/drops; Solution |
| Route | Ophthalmic; Inhalation, nebulizer; Inhalation |
| Strength | 300mg/5ml; 0.3% |
| Market Status | Tentative Approval; Prescription |
| Company | Teva Pharms Usa; Pulmoflow; Bausch And Lomb; Fera Pharms; Akorn |
| 11 of 12 | |
|---|---|
| Drug Name | Tobramycin sulfate |
| PubMed Health | Tobramycin and Dexamethasone (Ophthalmic route) |
| Drug Classes | Adrenal Glucocorticoid, Aminoglycoside, Aminoglycoside/Corticosteroid Combination |
| Drug Label | Tobramycin sulfate, a water-soluble antibiotic of the aminoglycoside group, is derived from the actinomycete Streptomyces tenebrarius. Tobramycin Injection USP is a clear and colorless sterile aqueous solution for parenteral administration.Tobramycin... |
| Active Ingredient | Tobramycin sulfate |
| Dosage Form | Injectable |
| Route | Injection |
| Strength | eq 40mg base/ml; eq 10mg base/ml; eq 1.2gm base/vial |
| Market Status | Prescription |
| Company | Hospira; X Gen Pharms; Teva Pharms Usa; Xellia Pharms Aps; Fresenius Kabi Usa; Hikma Maple; Agila Speclts; Akorn |
| 12 of 12 | |
|---|---|
| Drug Name | Tobrex |
| Active Ingredient | Tobramycin |
| Dosage Form | Solution/drops; Ointment |
| Route | Ophthalmic |
| Strength | 0.3% |
| Market Status | Prescription |
| Company | Alcon; Falcon Pharms |
Anti-Bacterial Agents
National Library of Medicine's Medical Subject Headings. Tobramycin. Online file (MeSH, 2016). Available from, as of December 5, 2016: https://www.nlm.nih.gov/mesh/2016/mesh_browser/MBrowser.html
/CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Tobramycin is included in the database.
NIH/NLM; ClinicalTrials.Gov. Available from, as of February 1, 2017: https://clinicaltrials.gov/ct2/results?term=TOBRAMYCIN&Search=Search
Tobramycin for Injection, USP is indicated for the treatment of serious bacterial infections caused by susceptible strains of the designated microorganisms in the diseases listed below: Septicemia in the pediatric patient and adult caused by Proteus aeruginosa, Enterobacter coli, and Klebsiella spp. Lower respiratory tract infections caused by P. aeruginosa, Klebsiella spp, Enterobacter spp, Serratia spp, E. coli, and S. aureus (penicillinase- and non-penicillinase-producing strains). Serious central-nervous-system infections (meningitis) caused by susceptible organisms. Intra-abdominal infections, including peritonitis, caused by E. coli, Klebsiella spp, and Enterobacter spp. Skin, bone, and skin structure infections caused by P. aeruginosa, Proteus spp, E. coli, Klebsiella spp, Enterobacter spp, and S. aureus. Complicated and recurrent urinary tract infections caused by P. aeruginosa, Proteus spp, (indole-positive and indole-negative), E. coli, Klebsiella spp, Enterobacter spp, Serratia spp, S. aureus, Providencia spp, and Citrobacter spp. /Included in US product labeling/
NIH; DailyMed. Current Medication Information for Tobramycin (Tobramycin Sulfate Injection, Powder, For Solution) (Updated: January 2016). Available from, as of February 13, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d62ff359-912b-4be1-9fc2-2dde8777eefb
Aminoglycosides, including tobramycin sulfate injection, USP are not indicated in uncomplicated initial episodes of urinary tract infections unless the causative organisms are not susceptible to antibiotics having less potential toxicity. Tobramycin for Injection, USP may be considered in serious staphylococcal infections when penicillin or other potentially less toxic drugs are contraindicated and when bacterial susceptibility testing and clinical judgment indicate its use.
NIH; DailyMed. Current Medication Information for Tobramycin (Tobramycin Sulfate Injection, Powder, For Solution) (Updated: January 2016). Available from, as of February 13, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d62ff359-912b-4be1-9fc2-2dde8777eefb
For more Therapeutic Uses (Complete) data for Tobramycin (9 total), please visit the HSDB record page.
/BOXED WARNING/ WARNINGS: Patients treated with tobramycin and other aminoglycosides should be under close clinical observation, because these drugs have an inherent potential for causing ototoxicity and nephrotoxicity. Neurotoxicity, manifested as both auditory and vestibular ototoxicity, can occur. The auditory changes are irreversible, are usually bilateral, and may be partial or total. Eighth-nerve impairment and nephrotoxicity may develop, primarily in patients having preexisting renal damage and in those with normal renal function to whom aminoglycosides are administered for longer periods or in higher doses than those recommended. Other manifestations of neurotoxicity may include numbness, skin tingling, muscle twitching, and convulsions. The risk of aminoglycoside-induced hearing loss increases with the degree of exposure to either high peak or high trough serum concentrations. Patients who develop cochlear damage may not have symptoms during therapy to warn them of eighth-nerve toxicity, and partial or total irreversible bilateral deafness may continue to develop after the drug has been discontinued. Rarely, nephrotoxicity may not become apparent until the first few days after cessation of therapy. Aminoglycoside-induced nephrotoxicity usually is reversible. Renal and eighth-nerve function should be closely monitored in patients with known or suspected renal impairment and also in those whose renal function is initially normal but who develop signs of renal dysfunction during therapy. Peak and trough serum concentrations of aminoglycosides should be monitored periodically during therapy to assure adequate levels and to avoid potentially toxic levels. Prolonged serum concentrations above 12 ug/mL should be avoided. Rising trough levels (above 2 mcg/mL) may indicate tissue accumulation. Such accumulation, excessive peak concentrations, advanced age, and cumulative dose may contribute to ototoxicity and nephrotoxicity. Urine should be examined for decreased specific gravity and increased excretion of protein, cells, and casts. Blood urea nitrogen, serum creatinine, and creatinine clearance should be measured periodically. When feasible, it is recommended that serial audiograms be obtained in patients old enough to be tested, particularly high-risk patients. Evidence of impairment of renal, vestibular, or auditory function requires discontinuation of the drug or dosage adjustment. Tobramycin should be used with caution in premature and neonatal infants because of their renal immaturity and the resulting prolongation of serum half-life of the drug. Concurrent and sequential use of other neurotoxic and/or nephrotoxic antibiotics, particularly other aminoglycosides (e.g., amikacin, streptomycin, neomycin, kanamycin, gentamicin, and paromomycin), cephaloridine, viomycin, polymyxin B, colistin, cisplatin, and vancomycin, should be avoided. Other factors that may increase patient risk are advanced age and dehydration. Aminoglycosides should not be given concurrently with potent diuretics, such as ethacrynic acid and furosemide. Some diuretics themselves cause ototoxicity, and intravenously administered diuretics enhance aminoglycoside toxicity by altering antibiotic concentrations in serum and tissue. Aminoglycosides can cause fetal harm when administered to a pregnant woman.
NIH; DailyMed. Current Medication Information for Tobramycin (Tobramycin Sulfate Injection, Powder, For Solution) (Updated: January 2016). Available from, as of February 13, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d62ff359-912b-4be1-9fc2-2dde8777eefb
Serious allergic reactions including anaphylaxis and dermatologic reactions including exfoliative dermatitis, toxic epidermal necrolysis, erythema multiforme, and Stevens-Johnson Syndrome have been reported rarely in patients on tobramycin therapy. Although rare, fatalities have been reported.
NIH; DailyMed. Current Medication Information for Tobramycin (Tobramycin Sulfate Injection, Powder, For Solution) (Updated: January 2016). Available from, as of February 13, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d62ff359-912b-4be1-9fc2-2dde8777eefb
Clostridium difficile associated diarrhea (CDAD) has been reported with use of nearly all antibacterial agents, including Tobramycin for Injection, USP, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the colon leading to overgrowth of C. difficile. C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin producing strains of C. difficile cause increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reported to occur over two months after the administration of antibacterial agents. If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically indicated.
NIH; DailyMed. Current Medication Information for Tobramycin (Tobramycin Sulfate Injection, Powder, For Solution) (Updated: January 2016). Available from, as of February 13, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d62ff359-912b-4be1-9fc2-2dde8777eefb
Adverse effects on both the vestibular and auditory branches of the eighth nerve have been noted, especially in patients receiving high doses or prolonged therapy, in those given previous courses of therapy with an ototoxin, and in cases of dehydration. Symptoms include dizziness, vertigo, tinnitus, roaring in the ears, and hearing loss. Hearing loss is usually irreversible and is manifested initially by diminution of high-tone acuity. Tobramycin and gentamicin sulfates closely parallel each other in regard to ototoxic potential.
NIH; DailyMed. Current Medication Information for Tobramycin (Tobramycin Sulfate Injection, Powder, For Solution) (Updated: January 2016). Available from, as of February 13, 2017: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=d62ff359-912b-4be1-9fc2-2dde8777eefb
For more Drug Warnings (Complete) data for Tobramycin (41 total), please visit the HSDB record page.
Inhaled tobramycin is indicated for the management of cystic fibrosis patients with _Pseudomonas aeruginosa_, but is not recommended in patients under six years of age, those with forced expiratory volume in 1 second (FEV1) <25 or >80% predicted, or in those with _Burkholderia cepacia_. Tobramycin applied topically to the eyes is indicated for the treatment of external eye (and adjoining structure) infections by susceptible bacteria. Tobramycin injection is indicated in adult and pediatric patients for the treatment of serious bacterial infections, including septicemia (caused by _P. aeruginosa_, _Escherichia coli_, and _Klebsiella_ spp.), lower respiratory tract infections (caused by _P. aeruginosa_, _Klebsiella_ spp., _Enterobacter_ spp., _Serratia_ spp., _E. coli_, and _Staphylococcus aureus_, both penicillinase and non-penicillinase-producing strains), serious central-nervous-system infections (meningitis, caused by susceptible organisms), intra-abdominal infections including peritonitis (caused by _E. coli_, _Klebsiella_ spp., and _Enterobacter_ spp.), skin, bone, and skin structure infections (caused by _P. aeruginosa_, _Proteus_ spp., _E. coli_, _Klebsiella_ spp., _Enterobacter_ spp., _Serratia_ spp. and _S. aureus_), and complicated and recurrent urinary tract infections (caused by _P. aeruginosa_, _Proteus_ spp., _E. coli_, _Klebsiella_ spp., _Enterobacter_ spp., _Serratia_ spp., _S. aureus_, _Providencia_ spp., and _Citrobacter_ spp.). Aminoglycosides, including tobramycin, should generally not be used in uncomplicated urinary tract infections or staphylococcal infections unless less toxic antibiotics cannot be used and the bacteria in question are known to be sensitive to aminoglycosides. As with all antibiotics, tobramycin use should be limited to cases where bacterial infections are known or strongly suspected to be caused by sensitive organisms, and the possible emergence of resistance should be monitored closely.
FDA Label
Tobi Podhaler is indicated for the suppressive therapy of chronic pulmonary infection due to Pseudomonas aeruginosa in adults and children aged 6 years and older with cystic fibrosis. See sections 4. 4 and 5. 1 regarding data in different age groups.
Consideration should be given to official guidance on the appropriate use of antibacterial agents.
Vantobra is indicated for the management of chronic pulmonary infection due to Pseudomonas aeruginosa in patients aged 6 years and older with cystic fibrosis (CF).
Consideration should be given to official guidance on the appropriate use of antibacterial agents.
Vantobra is indicated for the management of chronic pulmonary infection due to Pseudomonas aeruginosa in patients aged 6 years and older with cystic fibrosis (CF).
Consideration should be given to official guidance on the appropriate use of antibacterial agents.
Treatment of Pseudomonas aeruginosa pulmonary colonisation in patients with bronchiectasis
Treatment of Pseudomonas aeruginosa pulmonary infection / colonisation in patients with cystic fibrosis
Treatment of Pseudomonas aeruginosa pulmonary infection / colonisation in patients with cystic fibrosis
Tobramycin is an aminoglycoside antibiotic derived from the actinomycete _Streptomyces tenebrarius_. It has a broad spectrum of activity against Gram-negative bacteria, including _Enterobacteriaceae_, _Escherichia coli_, _Klebsiella pneumoniae_, _Morganella morganii_, _Moraxella lacunata_, _Proteus_ spp., _Haemophilus_ spp., _Acinetobacter_ spp., _Neisseria_ spp., and, importantly, _Pseudomonas aeruginosa_. Aminoglycosides also generally retain activity against the biothreat agents _Yersinia pestis_ and _Francisella tularensis_. In addition, aminoglycosides are active against some Gram-positive bacteria such as _Staphylococcus_ spp., including methicillin-resistant (MRSA) and vancomycin-resistant strains, _Streptococcus_ spp., and _Mycobacterium_ spp. Like other aminoglycosides, tobramycin is taken up and retained by proximal tubule and cochlear cells in the kidney and ear, respectively, and hence carries a risk of nephrotoxicity and ototoxicity. There is also a risk of neuromuscular block, which may be more pronounced in patients with preexisting neuromuscular disorders such as myasthenia gravis or Parkinson's disease. Aminoglycosides can cross the placenta, resulting in total, irreversible, bilateral congenital deafness in babies born to mothers who were administered an aminoglycoside during pregnancy. Due to the low systemic absorption of inhaled and topical tobramycin formulations, these effects are more pronounced with injected tobramycin than with other formulations. However, all formulations carry a risk of hypersensitivity reactions, including potentially fatal cutaneous reactions such as Stevens-Johnson syndrome and toxic epidermal necrolysis.
Anti-Bacterial Agents
Substances that inhibit the growth or reproduction of BACTERIA. (See all compounds classified as Anti-Bacterial Agents.)
J01GB01
J01GB01
J01GB01
J01GB01
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
J - Antiinfectives for systemic use
J01 - Antibacterials for systemic use
J01G - Aminoglycoside antibacterials
J01GB - Other aminoglycosides
J01GB01 - Tobramycin
S - Sensory organs
S01 - Ophthalmologicals
S01A - Antiinfectives
S01AA - Antibiotics
S01AA12 - Tobramycin
Absorption
Tobramycin administered by inhalation in cystic fibrosis patients showed greater variability in sputum as compared to serum. After a single 112 mg dose, the serum Cmax was 1.02 0.53 g/mL, which was reached in one hour (Tmax), while the sputum Cmax was 1048 1080 g/g. Comparatively, for a 300 mg dose, the serum Cmax was 1.04 0.58 g/mL, which was also reached within one hour, while the sputum Cmax was 737 1028 g/g. The systemic exposure (AUC0-12) was also similar between the two doses, at 4.6 2.0 gh/mL for the 112 mg dose and 4.8 2.5 gh/mL for the 300 mg dose. When tobramycin was administered over a four-week cycle at 112 mg twice daily, the Cmax measured one hour after dosing ranged from 1.48 0.69 g/mL to 1.99 0.59 g/mL.
Route of Elimination
Tobramycin is primarily excreted unchanged in the urine.
Volume of Distribution
Inhalation tobramycin had an apparent volume of distribution in the central compartment of 85.1 L for a typical cystic fibrosis patient.
Clearance
Inhaled tobramycin has an apparent serum clearance of 14.5 L/h in cystic fibrosis patients aged 6-58 years.
Tobramycin is poorly absorbed from the GI tract.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 43
Tobramycin is rapidly absorbed following IM administration. Following IM administration of a single dose of tobramycin of 1 mg/kg in adults with normal renal function, peak serum tobramycin concentrations average 4-6 ug/mL and are attained within 30-90 minutes; at 6-8 hours after the dose, serum concentrations are 1 ug/mL or less. When the same dose is administered by IV infusion over 30-60 minutes, similar plasma concentrations of the drug are attained.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 43
In one study in neonates receiving IM tobramycin in a dosage of 2 mg/kg every 12 hours, peak serum concentrations of the drug were attained 0.5-1 hour after a dose and ranged from 4.9-5.2 ug/mL after the first dose and 4.5-5.1 ug/mL after 10-16 doses. In neonates 2-7 days of age receiving tobramycin in a dosage of 2.5 mg/kg by IV infusion every 12 hours, steady-state peak serum concentrations ranged from 3.5-9.9 ug/mL and trough serum concentrations ranged from 1.1-3.6 ug/mL in those weighing less than 2 kg. In those weighing 2 kg or more, peak serum concentrations ranged from 5-10.2 ug/mL and trough serum concentrations ranged from 0.7-2 ug/mL.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 43
Bioavailability of tobramycin administered by oral inhalation via a nebulizer may be variable because of individual differences in nebulizer performance and airway pathology. Following oral inhalation via nebulization, tobramycin remains concentrated principally in the airways; the drug does not readily cross epithelial membranes. Tobramycin sputum concentrations are highly variable following oral inhalation, but the drug does not appear to accumulate in sputum following multiple doses. Following an initial 300-mg dose of commercially available tobramycin solution for oral inhalation given via a nebulizer, sputum concentrations of the drug at 10 minutes averaged 1237 ug/g (range: 35-7414 ug/g). After 20 weeks of intermittent therapy (300-mg twice daily for 28 days followed by 28 days without the drug), sputum concentrations 10 minutes after administration averaged 1154 ug/g (range: 39-8085 ug/g) and sputum concentrations 2 hours after administration were approximately 14% of those obtained 10 minutes after administration. Following a single 300-mg dose of the commercially available tobramycin solution for oral inhalation given via nebulization in patients with cystic fibrosis, serum tobramycin concentrations averaged 0.95 ug/mL at 1 hour after administration; after 20 weeks of intermittent therapy (300 mg twice daily for 28 days followed by 28 days without the drug), serum tobramycin concentrations averaged 1.05 ug/mL at 1 hour after administration.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 43
For more Absorption, Distribution and Excretion (Complete) data for Tobramycin (15 total), please visit the HSDB record page.
Tobramycin is not appreciably metabolized.
Aminoglycosides are not metabolized and are excreted unchanged in the urine primarily by glomerular filtration. /Aminoglycosides/
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 31
Tobramycin has an apparent serum terminal half-life of ~3 hours following a single 112 mg inhaled dose in cystic fibrosis patients.
Total body clearance of tobramycin is approximately 20% higher in patients with cystic fibrosis than in patients without the disease; however, renal clearance is similar.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 43
When tobramycin is administered by oral inhalation using a nebulizer, any drug that is not absorbed systemically probably is eliminated principally in expectorated sputum.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 43
... Terminal elimination half-lives of greater than 100 hours have been reported in adults with normal renal function following repeated IM or IV administration of the drug.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 43
The plasma elimination half-life of tobramycin following parenteral administration usually is 2-3 hours in adults with normal renal function and has ranged from 50-70 hours in adults with impaired renal function. The serum elimination half-life of tobramycin is reported to average 4.6 hours in full-term infants weighing more than 2.5 kg and 8.7 hours in infants weighing less than 1.5 kg. In one study in neonates 2-7 days of age, elimination half-life ranged from 5.68-13.6 hours in those weighing less than 2 kg and 3.54-6.73 hours in those weighing 2 kg or more.
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 43
Tobramycin is a 4,6-disubstituted 2-deoxystreptamine (DOS) ring-containing aminoglycoside antibiotic with activity against various Gram-negative and some Gram-positive bacteria. The mechanism of action of tobramycin has not been unambiguously elucidated, and some insights into its mechanism rely on results using similar aminoglycosides. In general, like other aminoglycosides, tobramycin is bactericidal and exhibits both immediate and delayed killing, which are attributed to different mechanisms, as outlined below. Aminoglycosides are polycationic at physiological pH, such that they readily bind to bacterial membranes ("ionic binding"); this includes binding to lipopolysaccharide and phospholipids within the outer membrane of Gram-negative bacteria and to teichoic acid and phospholipids within the cell membrane of Gram-positive bacteria. This binding displaces divalent cations and increases membrane permeability, which allows aminoglycoside entry. Additional aminoglycoside entry ("energy-dependent phase I") into the cytoplasm requires the proton-motive force, allowing access of the aminoglycoside to its primary intracellular target of the bacterial 30S ribosome. Mistranslated proteins produced as a result of aminoglycoside binding to the ribosome (see below) integrate into and disrupt the cell membrane, which allows more of the aminoglycoside into the cell ("energy-dependent phase II"). Hence, tobramycin and other aminoglycosides have both immediate bactericidal effects through membrane disruption and delayed bactericidal effects through impaired protein synthesis; observed experimental data and mathematical modelling support this two-mechanism model. Inhibition of protein synthesis was the first recognized effect of aminoglycoside antibiotics. Structural and cell biological studies suggest that aminoglycosides bind to the 16S rRNA in helix 44 (h44), near the A site of the 30S ribosomal subunit, altering interactions between h44 and h45. This binding also displaces two important residues, A1492 and A1493, from h44, mimicking normal conformational changes that occur with successful codon-anticodon pairing in the A site. Overall, aminoglycoside binding has several negative effects, including inhibiting translation initiation and elongation and ribosome recycling. Recent evidence suggests that the latter effect is due to a cryptic second binding site situated in h69 of the 23S rRNA of the 50S ribosomal subunit. Also, by stabilizing a conformation that mimics correct codon-anticodon pairing, aminoglycosides promote error-prone translation; mistranslated proteins can incorporate into the cell membrane, inducing the damage discussed above. Although direct mutation of the 16S rRNA is a rare resistance mechanism, due to the gene being present in numerous copies, posttranscriptional 16S rRNA modification by 16S rRNA methyltransferases (16S-RMTases) at the N7 position of G1405 or the N1 position of A1408 are common resistance mechanisms in aminoglycoside-resistant bacteria. These mutants also further support the proposed mechanism of action of aminoglycosides. Direct modification of the aminoglycoside itself through acetylation, adenylation, and phosphorylation by aminoglycoside-modifying enzymes (AMEs) are also commonly encountered resistance mutations. Finally, due to the requirement for active transport of aminoglycosides across bacterial membranes, they are not active against obligately anaerobic bacteria.
Aminoglycosides are usually bacterial in action. Although the exact mechanism of action has not been fully elucidated, the drugs appear to inhibit protein synthesis in susceptible bacteria by irreversibly binding to 30S ribosomal subunits. /Aminoglycosides/
American Society of Health-System Pharmacists 2016; Drug Information 2016. Bethesda, MD. 2016, p. 29
... Aminoglycosides are aminocyclitols that kill bacteria by inhibiting protein synthesis as they bind to the 16S rRNA and by disrupting the integrity of bacterial cell membrane. Aminoglycoside resistance mechanisms include: (a) the deactivation of aminoglycosides by N-acetylation, adenylylation or O-phosphorylation, (b) the reduction of the intracellular concentration of aminoglycosides by changes in outer membrane permeability, decreased inner membrane transport, active efflux, and drug trapping, (c) the alteration of the 30S ribosomal subunit target by mutation, and (d) methylation of the aminoglycoside binding site. ... /Aminoglycosides/
PMID:17657587 Shakil S et al; J Biomed Sci 15 (1): 5-14 (2008)