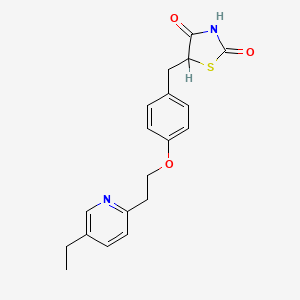
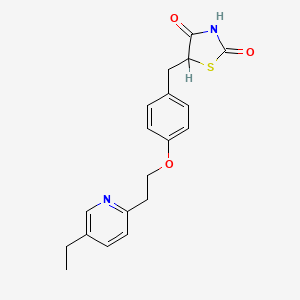
1. 5-(4-(2-(5-ethyl-2-pyridyl)ethoxy)benzyl)-2,4-thiazolidinedione
2. Actos
3. Ad 4833
4. Ad-4833
5. Ad4833
6. Pioglitazone Hydrochloride
7. U 72107a
8. U-72107a
9. U72,107a
10. U72107a
1. 111025-46-8
2. Glustin
3. Zactos
4. Pioglitazona
5. Pioglitazonum
6. Pioglitazonum [inn-latin]
7. Pioglitazona [inn-spanish]
8. 5-(4-(2-(5-ethylpyridin-2-yl)ethoxy)benzyl)thiazolidine-2,4-dione
9. Piozone
10. Pioglu
11. U 72107
12. Chebi:8228
13. Hsdb 7322
14. Unii-x4ov71u42s
15. X4ov71u42s
16. U-72107
17. 5-[4-[2-(5-ethyl-2-pyridyl)ethoxy]benzyl]-2,4-thiazolidinedione
18. 5-{4-[2-(5-ethylpyridin-2-yl)ethoxy]benzyl}-1,3-thiazolidine-2,4-dione
19. Dtxsid3037129
20. 5-(4-(2-(5-ethyl-2-pyridyl)ethoxy)benzyl)-2,4-thiazolidinedione
21. 5-[4-[2-(5-ethyl-2-pyridyl)ethoxy]benzyl]thiazolidine-2,4-dione
22. Pioglitazone (iarc)
23. Pioglitazone [iarc]
24. Pioglitazonum (inn-latin)
25. Pioglitazona (inn-spanish)
26. 5-(4-(2-(5-ethyl-2-pyridyl)ethoxy)benzyl)thiazolidine-2,4-dione
27. 5-{4-[2-(5-ethyl-2-pyridyl)ethoxy]benzyl}-2,4-thiazolidinedione
28. 5-(4-(2-(5-ethylpyridin-2-yl)ethoxy)benzyl)-1,3-thiazolidine-2,4-dione
29. Pioglitazonum (latin)
30. Dtxcid1017129
31. A10bg03
32. 2,4-thiazolidinedione, 5-((4-(2-(5-ethyl-2-pyridinyl)ethoxy)phenyl)methyl)-, (+-)-
33. (+-)-5-(p-(2-(5-ethyl-2-pyridyl)ethoxy)benzyl)-2,4-thiazolidinedione
34. Actos
35. 105355-27-9
36. Ad-4833
37. 5-[[4-[2-(5-ethylpyridin-2-yl)ethoxy]phenyl]methyl]-1,3-thiazolidine-2,4-dione
38. Pioglitazone (actos)
39. 5-[[4-[2-(5-ethyl-2-pyridinyl)ethoxy]phenyl]methyl]-2,4-thiazolidinedione
40. Pioglitazone (inn)
41. 105390-47-4
42. Mfcd00865504
43. Actos (tn)
44. 2,4-thiazolidinedione, 5-[[4-[2-(5-ethyl-2-pyridinyl)ethoxy]phenyl]methyl]-
45. 5-({4-[2-(5-ethylpyridin-2-yl)ethoxy]phenyl}methyl)-1,3-thiazolidine-2,4-dione
46. Pioglitazone [inn]
47. 5-((4-(2-(5-ethyl-2-pyridinyl)ethoxy)phenyl)methyl)-2,4-thiazolidinedione
48. Pioglitazone [ban:inn]
49. Pioglitazone [inn:ban]
50. 2,4-thiazolidinedione, 5-((4-(2-(5-ethyl-2-pyridinyl)ethoxy)phenyl)methyl)-
51. C19h20n2o3s
52. U-72107e
53. Pioglitazone?
54. Sr-01000763737
55. Pioglitazone Base
56. 2,4-thiazolidinedione, 5-[[4-[2-(5-ethyl-2-pyridinyl)ethoxy]phenyl]methyl]-, (+/-)-
57. [( Inverted Exclamation Marka)-5-[[4-[2-(5-ethyl-2-pyridinyl) Ethoxy] Phenyl] Methyl]-2,4-] Thiazolidinedione Monohydrochlorid
58. 2,4-thiazolidinedione, 5-((4-(2-(5-ethyl-2-pyridinyl)ethoxy)phenyl)methyl)-, (+/-)-
59. Pioglitazone-[d4]
60. Hs-0047
61. Spectrum_001623
62. Pioglitazone (standard)
63. Spectrum2_001679
64. Spectrum3_001002
65. Spectrum4_001130
66. Spectrum5_001480
67. Spectrum5_002067
68. Pioglitazone [mi]
69. Pioglitazone [hsdb]
70. Schembl4121
71. Pioglitazone [vandf]
72. Bspbio_002723
73. Kbiogr_001619
74. Kbioss_002103
75. Mls006011848
76. Pioglitazone [who-dd]
77. Spbio_001897
78. Gtpl2694
79. Pioglitazone [ema Epar]
80. Kbio2_002103
81. Kbio2_004671
82. Kbio2_007239
83. Kbio3_001943
84. Pioglitazone - Bio-x Trade Mark
85. Hyafethfcaujay-uhfffaoysa-n
86. Glxc-05211
87. Hms2089h14
88. Hms3651d09
89. Hms3712e16
90. Hms3884l10
91. Pharmakon1600-01504401
92. Bcp26474
93. Bbl029068
94. Bdbm50103521
95. Hb4139
96. Hy-13956r
97. Nsc758876
98. S2590
99. Stl309607
100. Stl373406
101. (+/-)-5-[p-[2-(ethyl-2-pyridyl)ethoxy]benzyl]-2,4-thiazolidinedione
102. Akos015894953
103. Akos022109420
104. Ac-1021
105. Ccg-220107
106. Cs-1700
107. Db01132
108. Fp39372
109. Sb17323
110. (+/-)-5-[[4-[2-(5-ethyl-2-pyridinyl)-ethoxy]phenyl]methyl]-2,4-thiazolidinedione
111. Ncgc00163128-01
112. Ncgc00163128-02
113. Ncgc00163128-03
114. Ncgc00163128-04
115. Ncgc00163128-05
116. Ncgc00163128-06
117. Ncgc00163128-07
118. Bp164273
119. Hy-13956
120. Smr002204015
121. Sy017473
122. Sbi-0206791.p001
123. Db-027350
124. Ns00000599
125. Sw197561-3
126. C07675
127. D08378
128. En300-117258
129. Ab00698454-10
130. Ab00698454_11
131. Ab00698454_12
132. Ab00698454_13
133. Q417765
134. Sr-01000763737-5
135. Brd-a48430263-001-07-7
136. Brd-a48430263-003-02-4
137. Brd-a48430263-003-06-5
138. Brd-a48430263-003-16-4
139. Brd-a48430263-003-17-2
140. Z1501480426
141. 5-[4-[2-(5-ethyl-2-pyridyl) Ethoxy]benzyl]-2,4-thiazolidinedione
142. 5-[4-[2-(5-ethyl-2-pyridyl)eth-oxy]benzyl]-2,4-thiazolidinedione
143. 5-{4-[2-(5-ethyl-2-pyridyl)ethoxy]benzyl}-2,4thiazolidinedione
144. 5-(4-(2-(5-ethylpyridin-2-yl)ethoxy)benzyl)-thiazolidine-2,4-dione
145. 5-[[4-[2-(5-ethyl-2-pyridyl)ethoxy] Phenyl]methyl]-2,4-thiazolidinedione
146. (+/-)-5-((4-(2-(5-ethyl-2-pyridinyl)ethoxy)phenyl)methyl)-2,4-thiazolidinedione
147. (+/-)-5-(p-(2-(5-ethyl-2-pyridyl)ethoxy)benzyl)-2,4-thiazolidinedione
148. (rs)-5-(4-(2-(5-ethylpyridin-2-yl)ethoxy)benzyl)thiazolidine-2,4-dione
149. 2,4-thiazolidinedione, 5-[[4-[2-(5-ethyl-2-pyridinyl)ethoxy]phenyl]methyl]- (9ci)
150. 5-[[4-[2-[(5-ethyl-2-pyridyl)]ethoxy]phenyl]methyl]thiazolidine- 2,4-dione
151. 5-{4-[2-(5-ethylpyridin-2-yl)ethoxy]benzyl}-4-hydroxy-1,3-thiazol-2(5h)-one
152. [()-5-[[4-[2-(5-ethyl-2-pyridinyl) Ethoxy] Phenyl] Methyl]-2,4-] Thiazolidinedione Monohydrochlorid
153. 198077-89-3
| Molecular Weight | 356.4 g/mol |
|---|---|
| Molecular Formula | C19H20N2O3S |
| XLogP3 | 3.8 |
| Hydrogen Bond Donor Count | 1 |
| Hydrogen Bond Acceptor Count | 5 |
| Rotatable Bond Count | 7 |
| Exact Mass | Da |
| Monoisotopic Mass | Da |
| Topological Polar Surface Area | 93.6 |
| Heavy Atom Count | 25 |
| Formal Charge | 0 |
| Complexity | 466 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 1 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Hypoglycemic Agents
National Library of Medicine's Medical Subject Headings. Pioglitazone. Online file (MeSH, 2018). Available from, as of January 22, 2018: https://meshb.nlm.nih.gov/search
/CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Pioglitazone is included in the database.
NIH/NLM; ClinicalTrials.Gov. Available from, as of January 22, 2018: https://clinicaltrials.gov/
Pioglitazone is used alone (monotherapy) or in combination with a sulfonylurea antidiabetic agent, metformin (either as a fixed-combination preparation or as individual drugs given concurrently), or insulin as an adjunct to diet and exercise for the management of type 2 diabetes mellitus. Pioglitazone is used also in fixed combination with glimepiride in patients with type 2 diabetes mellitus who are already receiving pioglitazone and a sulfonylurea separately or who are inadequately controlled on a sulfonylurea or pioglitazone alone. In patients whose hyperglycemia cannot be controlled with these other antidiabetic agents, pioglitazone should be added to, not substituted for, such antidiabetic therapy. /Included in US product labeling/
American Society of Health-System Pharmacists 2017; Drug Information 2017. Bethesda, MD. 2017, p. 3297
/EXPL THER/ Peroxisome proliferator activated receptor gamma-activating drugs show various salutary effects in preclinical models of neurodegenerative disease. The decade-long clinical usage of these drugs as antidiabetics now allows for evaluation of patient-oriented data sources. Using observational data from 2004-2010, we analyzed the association of pioglitazone and incidence of dementia in a prospective cohort study of 145,928 subjects aged >/= 60 years who, at baseline, were free of dementia and insulin-dependent diabetes mellitus. We distinguished between nondiabetics, diabetics without pioglitazone, diabetics with prescriptions of <8 calendar quarters of pioglitazone, and diabetics with =8 quarters. Cox proportional hazard models explored the relative risk (RR) of dementia incidence dependent on pioglitazone use adjusted for sex, age, use of rosiglitazone or metformin, and cardiovascular comorbidities. Long-term use of pioglitazone was associated with a lower dementia incidence. Relative to nondiabetics, the cumulative long-term use of pioglitazone reduced the dementia risk by 47% (RR=0.53, p=0.029). If diabetes patients used pioglitazone <8 quarters, the dementia risk was comparable to those of nondiabetics (RR=1.16, p=0.317), and diabetes patients without a pioglitazone treatment had a 23% increase in dementia risk (RR=1.23, p<0.001). We did not find evidence for age effects, nor for selection into pioglitazone treatment due to obesity. These findings indicate that pioglitazone treatment is associated with a reduced dementia risk in initially non-insulin-dependent diabetes mellitus patients. Prospective clinical trials are needed to evaluate a possible neuroprotective effect in these patients in an ageing population.
PMID:25974006 Heneka MT et al; Ann Neurol 78 (2): 284-94 (2015)
For more Therapeutic Uses (Complete) data for Pioglitazone (9 total), please visit the HSDB record page.
/BOXED WARNING/ WARNING: CONGESTIVE HEART FAILURE. Thiazolidinediones, including pioglitazone hydrochloride, cause or exacerbate congestive heart failure in some patients. After initiation of pioglitazone tablets, and after dose increases, monitor patients carefully for signs and symptoms of heart failure (e.g., excessive, rapid weight gain, dyspnea, and/or edema). If heart failure develops, it should be managed according to current standards of care and discontinuation or dose reduction of pioglitazone hydrochloride must be considered. Pioglitazone tablets are not recommended in patients with symptomatic heart failure. Initiation of pioglitazone hydrochloride in patients with established NYHA Class III or IV heart failure is contraindicated.
NIH; DailyMed. Current Medication Information for Pioglitazone Hydrochloride Tablet (Updated: December 27, 2017). Available from, as of January 26, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8f2d7000-37ca-4e09-98ec-07d1c0354cb3
Thiazolidinediones, including pioglitazone, alone or in combination with other antidiabetic agents, can cause fluid retention, which may lead to or exacerbate congestive heart failure (CHF). Use of thiazolidinediones is associated with an approximately twofold increased risk of CHF. Use of pioglitazone in combination with insulin or in patients with New York Heart Association (NYHA) class I or II heart failure may increase the risk. Patients should be observed for signs and symptoms of CHF (e.g., dyspnea, rapid weight gain, edema, unexplained cough or fatigue), especially during initiation of therapy and dosage titration. If signs and symptoms of CHF develop, the disorder should be managed according to current standards of care. In addition, a decrease in the dosage or discontinuance of pioglitazone must be considered in such patients.
American Society of Health-System Pharmacists 2017; Drug Information 2017. Bethesda, MD. 2017, p. 3298
Patients with New York Heart Association (NYHA) class III or IV cardiac status with or without congestive heart failure (CHF) or with an acute coronary event were not studied in clinical trials of pioglitazone; initiation of therapy with the drug is contraindicated in patients with NYHA class III or IV heart failure. Use of pioglitazone is not recommended in patients with symptomatic heart failure. Caution should be exercised in patients with edema and in those who are at risk for CHF. Thiazolidinedione therapy should not be initiated in hospitalized patients with diabetes mellitus because of the delayed onset of action and because possible drug-related increases in vascular volume and CHF may complicate care of patients with hemodynamic changes induced by coexisting conditions or in-hospital interventions.
American Society of Health-System Pharmacists 2017; Drug Information 2017. Bethesda, MD. 2017, p. 3298-9
Risk for pregnancy unless contraceptive measures initiated; anovulatory premenopausal women with insulin resistance may resume ovulation during therapy. The frequency of resumption of ovulation with pioglitazone therapy has not been evaluated in clinical studies, and, therefore, is unknown. If menstrual dysfunction occurs, weigh risks versus benefits of continued pioglitazone.
American Society of Health-System Pharmacists 2017; Drug Information 2017. Bethesda, MD. 2017, p. 3299
For more Drug Warnings (Complete) data for Pioglitazone (20 total), please visit the HSDB record page.
Pioglitazone is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. It is also available in combination with [metformin], [glimepiride], or [alogliptin] for the same indication.
FDA Label
Pioglitazone is indicated in the treatment of type-2 diabetes mellitus: as monotherapy: in patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance; as dual oral therapy in combination with: metformin, in patients (particularly overweight patients) with insufficient glycaemic control despite maximal tolerated dose of monotherapy with metformin; a sulphonylurea, only in patients who show intolerance to metformin or for whom metformin is contraindicated, with insufficient glycaemic control despite maximal tolerated dose of monotherapy with a sulphonylurea; as triple oral therapy in combination with: metformin and a sulphonylurea, in patients (particularly overweight patients) with insufficient glycaemic control despite dual oral therapy. Pioglitazone is also indicated for combination with insulin in type-2 diabetes mellitus patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance.
Pioglitazone is indicated as second or third line treatment of type 2 diabetes mellitus as described below: as monotherapyin adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance. as dual oral therapy in combination withmetformin, in adult patients (particularly overweight patients) with insufficient glycaemic control despite maximal tolerated dose of monotherapy with metformin. a sulphonylurea, only in adult patients who show intolerance to metformin or for whom metformin is contraindicated, with insufficient glycaemic control despite maximal tolerated dose of monotherapy with a sulphonylurea. as triple oral therapy in combination withmetformin and a sulphonylurea, in adult patients (particularly overweight patients) with insufficient glycaemic control despite dual oral therapy. Pioglitazone is also indicated for combination with insulin in type 2 diabetes mellitus adult patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance (see section 4. 4). After initiation of therapy with pioglitazone, patients should be reviewed after 3 to 6 months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained (see section 4. 4).
Pioglitazone is indicated in the treatment of type 2 diabetes mellitus: as monotherapy- in adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intoleranceas dual oral therapy in combination with- metformin, in adult patients (particularly overweight patients) with insufficient glycaemic control despite maximal tolerated dose of monotherapy with metformin- a sulphonylurea, only in adult patients who show intolerance to metformin or for whom metformin is contraindicated, with insufficient glycaemic control despite maximal tolerated dose of monotherapy with a sulphonylureaas triple oral therapy in combination with- metformin and a sulphonylurea, in adult patients (particularly overweight patients) with insufficient glycaemic control despite dual oral therapy. Pioglitazone is also indicated for combination with insulin in type 2 diabetes mellitus adult patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance. After initiation of therapy with pioglitazone, patients should be reviewed after 3 to 6 months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained.
Pioglitazone is indicated as second or third line treatment of type-2 diabetes mellitus as described below: as monotherapy: in adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance; as dual oral therapy in combination with: metformin, in adult patients (particularly overweight patients) with insufficient glycaemic control despite maximal tolerated dose of monotherapy with metformin; a sulphonylurea, only in adult patients who show intolerance to metformin or for whom metformin is contraindicated, with insufficient glycaemic control despite maximal tolerated dose of monotherapy with a sulphonylurea; as triple oral therapy in combination with: metformin and a sulphonylurea, in adult patients (particularly overweight patients) with insufficient glycaemic control despite dual oral therapy. Pioglitazone is also indicated for combination with insulin in type-2 diabetes mellitus adult patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance. After initiation of therapy with pioglitazone, patients should be reviewed after 3 to 6 months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained.
Pioglitazone is indicated as second or third line treatment of type-2 diabetes mellitus as described below: as monotherapy: in adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance. as dual oral therapy in combination with: metformin, in adult patients (particularly overweight patients) with insufficient glycaemic control despite maximal tolerated dose of monotherapy with metformin; a sulphonylurea, only in adult patients who show intolerance to metformin or for whom metformin is contraindicated, with insufficient glycaemic control despite maximal tolerated dose of monotherapy with a sulphonylurea; as triple oral therapy in combination with: metformin and a sulphonylurea, in adult patients (particularly overweight patients) with insufficient glycaemic control despite dual oral therapy. Pioglitazone is also indicated for combination with insulin in type-2 diabetes mellitus adult patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance. After initiation of therapy with pioglitazone, patients should be reviewed after three to six months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained.
Pioglitazone is indicated in the treatment of type-2 diabetes mellitus as monotherapy: , , , in adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance. , , , Pioglitazone is also indicated for combination with insulin in type 2 diabetes mellitus adult patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance. , , After initiation of therapy with pioglitazone, patients should be reviewed after 3 to 6 months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained. ,
Pioglitazone is indicated in the treatment of type-2 diabetes mellitus: as monotherapyin adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance. After initiation of therapy with pioglitazone, patients should be reviewed after 3 to 6 months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained.
Pioglitazone is indicated as second or third line treatment of type 2 diabetes mellitus as described below: as monotherapyin adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance; as dual oral therapy in combination withmetformin, in adult patients (particularly overweight patients) with insufficient glycaemic control despite maximal tolerated dose of monotherapy with metformin; a sulphonylurea, only in adult patients who show intolerance to metformin or for whom metformin is contraindicated, with insufficient glycaemic control despite maximal tolerated dose of monotherapy with a sulphonylurea; as triple oral therapy in combination withmetformin and a sulphonylurea, in adult patients (particularly overweight patients) with insufficient glycaemic control despite dual oral therapy. Pioglitazone is also indicated for combination with insulin in type 2 diabetes mellitus in adult patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance. After initiation of therapy with pioglitazone, patients should be reviewed after 3 to 6 months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained.
Pioglitazone is indicated as second or third line treatment of type 2 diabetes mellitus as described below: as monotherapy- in adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance; as dual oral therapy in combination with- a sulphonylurea, only in adult patients who show intolerance to metformin or for whom metformin is contraindicated, with insufficient glycaemic control despite maximal tolerated dose of monotherapy with a sulphonylurea; Pioglitazone is also indicated for combination with insulin in type 2 diabetes mellitus in adult patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance. After initiation of therapy with pioglitazone, patients should be reviewed after 3 to 6 months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained.
Pioglitazone is indicated as second- or third-line treatment of type-2 diabetes mellitus as described below: as monotherapy: in adult patients (particularly overweight patients) inadequately controlled by diet and exercise for whom metformin is inappropriate because of contraindications or intolerance; as dual oral therapy in combination with: metformin, in adult patients (particularly overweight patients) with insufficient glycaemic control despite maximal tolerated dose of monotherapy with metformin; a sulphonylurea, only in adult patients who show intolerance to metformin or for whom metformin is contraindicated, with insufficient glycaemic control despite maximal tolerated dose of monotherapy with a sulphonylurea; as triple oral therapy in combination with: metformin and a sulphonylurea, in adult patients (particularly overweight patients) with insufficient glycaemic control despite dual oral therapy. Pioglitazone is also indicated for combination with insulin in type-2-diabetes-mellitus adult patients with insufficient glycaemic control on insulin for whom metformin is inappropriate because of contraindications or intolerance (see section 4. 4). After initiation of therapy with pioglitazone, patients should be reviewed after three to six months to assess adequacy of response to treatment (e. g. reduction in HbA1c). In patients who fail to show an adequate response, pioglitazone should be discontinued. In light of potential risks with prolonged therapy, prescribers should confirm at subsequent routine reviews that the benefit of pioglitazone is maintained (see section 4. 4).
Pioglitazone is an oral antidiabetic from the thiazolidinedione drug class, FDA approved for treating type 2 diabetes mellitus in adults, as an adjunct to diet and exercise.
Hypoglycemic Agents
Substances which lower blood glucose levels. (See all compounds classified as Hypoglycemic Agents.)
A10BG03
A10BG03
A10BG03
A10BG03
A10BG03
A10BG03
A10BG03
A10BG03
A10BG03
A10BG03
A10BG03
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
A - Alimentary tract and metabolism
A10 - Drugs used in diabetes
A10B - Blood glucose lowering drugs, excl. insulins
A10BG - Thiazolidinediones
A10BG03 - Pioglitazone
Absorption
Following oral administration of pioglitazone, peak serum concentrations are observed within 2 hours (Tmax) - food slightly delays the time to peak serum concentration, increasing Tmax to approximately 3-4 hours, but does not alter the extent of absorption. Steady-state concentrations of both parent drug and its primary active metabolites are achieved after 7 days of once-daily administration of pioglitazone. Cmax and AUC increase proportionately to administered doses.
Route of Elimination
Approximately 15-30% of orally administered pioglitazone is recovered in the urine. The bulk of its elimination, then, is presumed to be through the excretion of unchanged drug in the bile or as metabolites in the feces.
Volume of Distribution
The average apparent volume of distribution of pioglitazone is 0.63 0.41 L/kg.
Clearance
The apparent clearance of orally administered pioglitazone is 5-7 L/h.
There was no significant difference in the pharmacokinetic profile of pioglitazone in subjects with normal or with moderately impaired renal function. In patients with moderate and severe renal impairment, although mean serum concentrations of pioglitazone and its metabolites were increased, no dose adjustment is needed. After repeated oral doses of pioglitazone, mean AUC values were decreased in patients with severe renal impairment compared with healthy subjects with normal renal function for pioglitazone.
IARC. Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. Geneva: World Health Organization, International Agency for Research on Cancer, 1972-PRESENT. (Multivolume work). Available at: https://monographs.iarc.fr/ENG/Classification/index.php, p. V108 362 (2016)
Following oral administration, approximately 15% to 30% of the pioglitazone dose is recovered in the urine. Renal elimination of pioglitazone is negligible, and the drug is excreted primarily as metabolites and their conjugates. It is presumed that most of the oral dose is excreted into the bile either unchanged or as metabolites and eliminated in the feces.
NIH; DailyMed. Current Medication Information for Pioglitazone Hydrochloride Tablet (Updated: December 27, 2017). Available from, as of January 26, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8f2d7000-37ca-4e09-98ec-07d1c0354cb3
Pioglitazone is a thiazolidinedione insulin sensitizer that has shown efficacy in Type 2 diabetes and nonalcoholic fatty liver disease in humans. It may be useful for treatment of similar conditions in cats. The purpose of this study was to investigate the pharmacokinetics of pioglitazone in lean and obese cats, to provide a foundation for assessment of its effects on insulin sensitivity and lipid metabolism. Pioglitazone was administered intravenously (median 0.2 mg/kg) or orally (3 mg/kg) to 6 healthy lean (3.96 +/- 0.56 kg) and 6 obese (6.43 +/- 0.48 kg) cats, in a two by two Latin Square design with a 4-week washout period. Blood samples were collected over 24 hr, and pioglitazone concentrations were measured via a validated high-performance liquid chromatography assay. Pharmacokinetic parameters were determined using two-compartmental analysis for IV data and noncompartmental analysis for oral data. After oral administration, mean bioavailability was 55%, t(1/2) was 3.5 h, T(max) was 3.6 hr, C(max) was 2131 ng/mL, and AUC(0-8) was 15,56 ng/mL/hr. There were no statistically significant differences in pharmacokinetic parameters between lean and obese cats following either oral or intravenous administration. Systemic exposure to pioglitazone in cats after a 3 mg/kg oral dose approximates that observed in humans with therapeutic doses.
PMID:22612529 Clark MH et al; J Vet Pharmacol Ther 35 (5): 428-36 (2012)
The mean apparent volume of distribution (Vd/F) of pioglitazone following single-dose administration is 0.63 +/- 0.41 (mean +/- SD) L/kg of body weight. Pioglitazone is extensively protein bound (> 99%) in human serum, principally to serum albumin. Pioglitazone also binds to other serum proteins, but with lower affinity. M-III (keto derivative of pioglitazone) and M-IV (hydroxyl derivative of pioglitazone) are also extensively bound (> 98%) to serum albumin.
NIH; DailyMed. Current Medication Information for Pioglitazone Hydrochloride Tablet (Updated: December 27, 2017). Available from, as of January 26, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8f2d7000-37ca-4e09-98ec-07d1c0354cb3
For more Absorption, Distribution and Excretion (Complete) data for Pioglitazone (6 total), please visit the HSDB record page.
Pioglitazone is extensively metabolized by both hydroxylation and oxidation - the resulting metabolites are also partly converted to glucuronide or sulfate conjugates. The pharmacologically active M-IV and M-III metabolites are the main metabolites found in human serum and their circulating concentrations are equal to, or greater than, those of the parent drug. The specific CYP isoenzymes involved in the metabolism of pioglitazone are CYP2C8 and, to a lesser degree, CYP3A4. There is also some evidence to suggest a contribution by extrahepatic CYP1A1.
Isoforms of cytochrome P450 (CYP) are involved in the metabolism of pioglitazone, including CYP2C8 and, to a lesser degree, CYP3A4. CYP2C9 is not significantly involved in the elimination of pioglitazone. Pioglitazone is not a strong inducer of CYP3A4, and pioglitazone was not shown to induce CYPs.
IARC. Monographs on the Evaluation of the Carcinogenic Risk of Chemicals to Humans. Geneva: World Health Organization, International Agency for Research on Cancer, 1972-PRESENT. (Multivolume work). Available at: https://monographs.iarc.fr/ENG/Classification/index.php, p. V108 362 (2016)
Pioglitazone is extensively metabolized by hydroxylation and oxidation; the metabolites also partly convert to glucuronide or sulfate conjugates. Metabolites M-III (keto derivative of pioglitazone) and M-IV (hydroxyl derivative of pioglitazone) are the major circulating active metabolites in humans.
NIH; DailyMed. Current Medication Information for Pioglitazone Hydrochloride Tablet (Updated: December 27, 2017). Available from, as of January 26, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8f2d7000-37ca-4e09-98ec-07d1c0354cb3
Pioglitazone has known human metabolites that include 5-({4-[2-(5-ethylpyridin-2-yl)-2-hydroxyethoxy]phenyl}methyl)-1,3-thiazolidine-2,4-dione, 2-[6-(2-{4-[(2,4-dioxo-1,3-thiazolidin-5-yl)methyl]phenoxy}ethyl)pyridin-3-yl]acetic acid, and 5-[(4-{2-[5-(1-hydroxyethyl)pyridin-2-yl]ethoxy}phenyl)methyl]-1,3-thiazolidine-2,4-dione.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
Hepatic
The mean serum half-life of pioglitazone and its metabolites (M-III and M-IV) range from 3-7 hours and 16-24 hours, respectively.
The mean serum half-life of pioglitazone and its metabolites (M-III and M-IV) range from three to seven hours and 16 to 24 hours, respectively.
NIH; DailyMed. Current Medication Information for Pioglitazone Hydrochloride Tablet (Updated: December 27, 2017). Available from, as of January 26, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8f2d7000-37ca-4e09-98ec-07d1c0354cb3
Pioglitazone is a selective agonist at peroxisome proliferator-activated receptor-gamma (PPAR) in target tissues for insulin action such as adipose tissue, skeletal muscle, and liver. Activation of PPAR increases the transcription of insulin-responsive genes involved in the control of glucose and lipid production, transport, and utilization. Through this mechanism, pioglitazone both enhances tissue sensitivity to insulin and reduces the hepatic production of glucose (i.e. gluconeogenesis) - insulin resistance associated with type 2 diabetes mellitus is therefore improved without an increase in insulin secretion by pancreatic beta cells.
Repeated administration of peroxisome proliferator-activated receptor gamma (PPARgamma) agonists reduces neuropathic pain-like behavior and associated changes in glial activation in the spinal cord dorsal horn. As PPARgamma is a nuclear receptor, sustained changes in gene expression are widely believed to be the mechanism of pain reduction. However, we recently reported that a single intrathecal (i.t.) injection of pioglitazone, a PPARgamma agonist, reduced hyperalgesia within 30 minutes, a time frame that is typically less than that required for genomic mechanisms. To determine the very rapid antihyperalgesic actions of PPARgamma activation, we administered pioglitazone to rats with spared nerve injury and evaluated hyperalgesia. Pioglitazone inhibited hyperalgesia within 5 minutes of injection, consistent with a nongenomic mechanism. Systemic or i.t. administration of GW9662, a PPARgamma antagonist, inhibited the antihyperalgesic actions of intraperitoneal or i.t. pioglitazone, suggesting a spinal PPAR?-dependent mechanism. To further address the contribution of nongenomic mechanisms, we blocked new protein synthesis in the spinal cord with anisomycin. When coadministered intrathecally, anisomycin did not change pioglitazone antihyperalgesia at an early 7.5-minute time point, further supporting a rapid nongenomic mechanism. At later time points, anisomycin reduced pioglitazone antihyperalgesia, suggesting delayed recruitment of genomic mechanisms. Pioglitazone reduction of spared nerve injury-induced increases in GFAP expression occurred more rapidly than expected, within 60 minutes. We are the first to show that activation of spinal PPARgamma rapidly reduces neuropathic pain independent of canonical genomic activity. We conclude that acute pioglitazone inhibits neuropathic pain in part by reducing astrocyte activation and through both genomic and nongenomic PPARgamma mechanisms.
PMID:25599238 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4329091 Griggs RB et al; Pain 156 (3): 469-82 (2015)
Pioglitazone hydrochloride is a thiazolidinedione that depends on the presence of insulin for its mechanism of action. Pioglitazone hydrochloride decreases insulin resistance in the periphery and in the liver resulting in increased insulin-dependent glucose disposal and decreased hepatic glucose output. Pioglitazone is not an insulin secretagogue. Pioglitazone is an agonist for peroxisome proliferator-activated receptor-gamma (PPARgamma). PPAR receptors are found in tissues important for insulin action such as adipose tissue, skeletal muscle, and liver. Activation of PPARgamma nuclear receptors modulates the transcription of a number of insulin responsive genes involved in the control of glucose and lipid metabolism.
NIH; DailyMed. Current Medication Information for Pioglitazone Hydrochloride Tablet (Updated: December 27, 2017). Available from, as of January 26, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=8f2d7000-37ca-4e09-98ec-07d1c0354cb3
... Thiazolidinediones reduce insulin resistance not only in type 2 diabetes but also in non-diabetic conditions associated with insulin resistance such as obesity. The mechanism of action involves binding to the peroxisome proliferator-activated receptor (PPAR)gamma, a transcription factor that regulates the expression of specific genes especially in fat cells but also in other tissues. It is likely that thiazolidinediones primarily act in adipose tissue where PPARgamma is predominantly expressed. Thiazolidinediones have been shown to interfere with expression and release of mediators of insulin resistance originating in adipose tissue (e.g. free fatty acids, adipocytokines such as tumor necrosis factor alpha, resistin, adiponectin) in a way that results in net improvement of insulin sensitivity (i.e. in muscle and liver). Nevertheless, a direct molecular effect in skeletal muscle cannot be excluded. ...
PMID:12173692 Stumvoll M, Haring HU; Ann Med 34 (3): 217-24 (2002)
Pioglitazone, a full peroxisome proliferator-activated receptor (PPAR)-gamma agonist, improves insulin sensitivity by increasing circulating adiponectin levels. However, the molecular mechanisms by which pioglitazone induces insulin sensitization are not fully understood. In this study, we investigated whether pioglitazone improves insulin resistance via upregulation of either 2 distinct receptors for adiponectin (AdipoR1 or AdipoR2) expression in 3T3-L1 adipocytes. Glucose uptake was evaluated by 2-[(3)H] deoxy-glucose uptake assay in 3T3-L1 adipocytes with pioglitazone treatment. AdipoR1 and AdipoR2 mRNA expressions were analyzed by qRT-PCR. /The investigators/ first confirmed that pioglitazone significantly increased insulin-induced 2-deoxyglucose (2-DOG) uptake in 3T3-L1 adipocytes. Next, we investigated the mRNA expression and regulation of AdipoR1 and AdipoR2 after treatment with pioglitazone. Interestingly, pioglitazone significantly induced AdipoR2 expression but it did not affect AdipoR1 expression. In addition, adenovirus-mediated PPARgamma expression significantly enhanced the effects of pioglitazone on insulin-stimulated 2-DOG uptake and AdipoR2 expression in 3T3-L1 adipocytes. These data suggest that pioglitazone enhances adiponectin's autocrine and paracrine actions in 3T3-L1 adipocytes via upregulation of PPARgamma-mediated AdipoR2 expression. Furthermore, we found that pioglitazone significantly increased AMP-activated protein kinase (AMPK) phosphorylation in insulin-stimulated 3T3-L1 adipocytes, but it did not lead to the phosphorylation of IRS-1, Akt, or protein kinase ... Pioglitazone increases insulin sensitivity, at least partly, by PPARgamma-AdipoR2-mediated AMPK phosphorylation in 3T3-L1 adipocytes. In conclusion, the upregulation of AdipoR2 expression may be one of the mechanisms by which pioglitazone improves insulin resistance in 3T3-L1 adipocytes.
PMID:21514306 Kudoh A et al; Life Sci 88 (23-24): 1055-62 (2011)
For more Mechanism of Action (Complete) data for Pioglitazone (6 total), please visit the HSDB record page.