

API Suppliers

US DMFs Filed

CEP/COS Certifications
0

JDMFs Filed
0
Other Certificates
Other Suppliers
0

USA (Orange Book)

Europe
0

Canada
0

Australia
0

South Africa
0
Uploaded Dossiers
0
U.S. Medicaid
0
Annual Reports
0
0
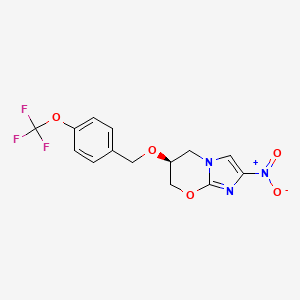
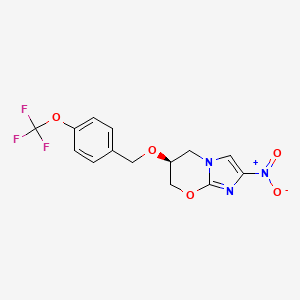
1. 2-nitro-6-(4-(trifluoromethoxy)benzyloxy)-6,7-dihydro-5h-imidazo(2,1-b)(1,3)oxazine
2. Pa 824
3. Pa-824
4. Pa824 Cpd
1. Pa-824
2. 187235-37-6
3. Pa 824
4. Pa824
5. (s)-2-nitro-6-((4-(trifluoromethoxy)benzyl)oxy)-6,7-dihydro-5h-imidazo[2,1-b][1,3]oxazine
6. (s)-pa 824
7. 2xoi31yc4n
8. Chembl227875
9. Mmv688755
10. (6s)-2-nitro-6-[[4-(trifluoromethoxy)phenyl]methoxy]-6,7-dihydro-5h-imidazo[2,1-b][1,3]oxazine
11. (6s)-2-nitro-6-{[4-(trifluoromethoxy)benzyl]oxy}-6,7-dihydro-5h-imidazo[2,1-b][1,3]oxazine
12. (6s)-2-nitro-6-{[4-(trifluoromethoxy)phenyl]methoxy}-5h,6h,7h-imidazo[2,1-b][1,3]oxazine
13. Pretomanid [usan:inn]
14. Unii-2xoi31yc4n
15. Pretomanid (tn)
16. Pa-824(pretomanid)
17. Pretomanid [mi]
18. Pretomanid [inn]
19. Pretomanid (usan/inn)
20. Pretomanid [usan]
21. Pretomanid [who-dd]
22. Mls006011141
23. Schembl2983011
24. Dtxsid8041163
25. Pretomanid [orange Book]
26. Gtpl11172
27. Ex-a1749
28. Zinc3821675
29. Bdbm50363237
30. Cs1245
31. Mfcd06809939
32. S1162
33. Akos024464713
34. Ccg-268145
35. Db05154
36. Ds-7321
37. 2-nitro-6-(4-(trifluoromethoxy)benzyloxy)-6,7-dihydro-5h-imidazo(2,1-b)(1,3)oxazine
38. Ncgc00346682-01
39. Ncgc00346682-02
40. Ac-25501
41. Hy-10844
42. Smr004702918
43. P2718
44. Sw220281-1
45. D10722
46. A855886
47. Sr-05000022748
48. Q7118312
49. Sr-05000022748-1
50. (3s)-3-(4-trifluoromethoxybenzyloxy)-6-nitro-2h-3,4-dihydroimidazo(2,1-b)oxazine
51. (s)-2-nitro-6-(4-(trifluoromethoxy)benzyloxy)-6,7-dihydro-5h-imidazo(2,1-b)(1,3)oxazine
52. {4-[((3s)-6-nitro(2h,3h,4h-imidazolo[2,1-b]1,3-oxazaperhydroin-3-yloxy))methyl]phenoxy}trifluoromethane
53. 5h-imidazo(2,1-b)(1,3)oxazine, 6,7-dihydro-2-nitro-6-((4-(trifluoromethoxy)phenyl)methoxy)-, (6s)-
54. Pretomanid;(6s)-6,7-dihydro-2-nitro-6-[[4-(trifluoromethoxy)phenyl]methoxy]-5h-imidazo[2,1-b][1,3]oxazine
| Molecular Weight | 359.26 g/mol |
|---|---|
| Molecular Formula | C14H12F3N3O5 |
| XLogP3 | 2.8 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 9 |
| Rotatable Bond Count | 4 |
| Exact Mass | 359.07290498 g/mol |
| Monoisotopic Mass | 359.07290498 g/mol |
| Topological Polar Surface Area | 91.3 Ų |
| Heavy Atom Count | 25 |
| Formal Charge | 0 |
| Complexity | 468 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 1 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Pretomanid is indicated for adults in combination with bedaquiline and linezolid for the treatment of pulmonary forms of nonresponsive multidrug-resistant (MDR), extensively drug-resistant (XDR), and treatment-intolerant forms of pulmonary tuberculosis (TB). It is important to note that the following conditions are not approved indications for pretomanid therapy, according to the FDA: Drug-sensitive (DS) tuberculosis, latent tuberculosis caused by M.tuberculosis, extra-pulmonary tuberculosis caused by M.tuberculosis, and multidrug-resistant TB that is not treatment-intolerant or nonresponsive to conventional TB therapy.
Dovprela is indicated in combination with bedaquiline and linezolid, in adults, for the treatment of pulmonary extensively drug resistant (XDR), or treatment-intolerant or nonresponsive multidrug-resistant (MDR) tuberculosis (TB).
Consideration should be given to official guidance on the appropriate use of antibacterial agents.
Treatment of multi-drug-resistant tuberculosis
Pretomanid kills the actively replicating bacteria causing tuberculosis, known as Mycobacterium tuberculosis, and shortens the duration of treatment in patients who suffer from resistant forms of pulmonary TB by killing dormant bacteria. In rodent models of tuberculosis infection, pretomanid administered in a regimen with bedaquiline and linezolid caused a significant reduction in pulmonary bacterial cell counts. A decrease in the frequency of TB relapses at 2 and 3 months after treatment was observed after the administration of this regimen, when compared to the administration of a 2-drug regimen. Successful outcomes have been recorded for patients with XDR and MDR following a clinical trial of the pretomanid regimen, demonstrating a 90% cure rate after 6 months. **A note on cardiac QT prolongation, hepatotoxicity, and myelosuppression** This drug has the propensity to caused cardiac QT interval prolongation and significant hepatotoxicity, as well as myelosuppression. Caution must be observed during the administration of this drug.
J04
J - Antiinfectives for systemic use
J04 - Antimycobacterials
J04A - Drugs for treatment of tuberculosis
J04AK - Other drugs for treatment of tuberculosis
J04AK08 - Pretomanid
Absorption
This drug is absorbed in the gastrointestinal tract. The steady-state Cmax of pretomanid was estimated to be 1.7 g/mL after a single 200mg oral dose. In a separate pharmacokinetic modeling study, the Cmax of a 200mg dose was 1.1 g/ml. Tmax in a study of healthy subjects in the fed or unfed state was achieved within 4 to 5 hours. The AUC in the same study was found to be about 28.1 ghr/mL in the fasted state and about 51.6 ghr/mL in the fed state, showing higher absorption when taken with high-calorie and high-fat food.
Route of Elimination
Healthy adult male volunteers were administered a 1,100 mg oral dose of radiolabeled pretomanid in one pharmacokinetic study. An average of about 53% of the radioactive dose was found to be excreted in the urine. Approximately 38% was measured mainly as metabolites in the feces. A estimated 1% of the radiolabeled dose was measured as unchanged drug in the urine.
Volume of Distribution
A pharmacokinetic modeling study estimated the volume of distribution at 130 5L. A pharmacokinetic study in healthy volunteers determined a volume of distribution of about 180 51.3L in fasted state and 97.0 17.2L in the fed state.
Clearance
The clearance of pretomanid in a pharmacokinetic simulation study has been estimated at 4.8 0.2 liters/h. According to the FDA label, the clearance of a single 200 mg oral dose of pretomanid is estimated to be 7.6 liters/h in the fasted state, and 3.9 liters/h in the fed state.
Various reductive and oxidative pathways are responsible for pretomanid metabolism, with no single major metabolic pathway identified. According to in vitro studies, CYP3A4 is responsible for a 20% contribution to the metabolism of pretomanid.
The elimination half-life was determined to be 16.9-17.4 hours in a pharmacokinetic study of healthy subjects. An FDA briefing document reports a half-life of 18 hours.
Pretomanid is a prodrug which is metabolically activated by a nitroreductase enzyme, known as Ddn, producing various active metabolites that are responsible for its other therapeutic actions, particularly the induction of nitric oxide. The nitroreductase enzyme which activates pretomanid is deazaflavin dependent and relies on reduced cofactor F420. Reduction of F420 occurs via the enzyme glucose-6-phosphate dehydrogenase. Reduction of pretomanid's imidazole ring at the C-3 position causes the formation of the metabolites, which include a des-nitro derivative. The formation of this derivative leads to increased levels of nitric oxide, leading to bactericidal activities under anaerobic conditions via its action as a bacterial respiratory poison. Bactericidal activity against anaerobes is reported to be associated with a shortened duration of antibiotic treatment. Pretomanid exerts aerobic bactericidal effects through its inhibitory actions on bacterial cell wall mycolic acid biosynthesis. This allows for the killing of actively replicating Mycobacterium tuberculosis bacteria, resulting in the treatment of active tuberculosis infection. The molecular mechanism of the above bactericidal effects is poorly understood at this time, but may involve effects exerted on various genes that affect the cell wall, including the fasI and fasII as well as the efpA and iniBAC operons. Other possible targets include the genes of the cyd operon. The clinical effects of the above target relations are unknown at this time.


