


API Suppliers

US DMFs Filed

CEP/COS Certifications
0

JDMFs Filed
Other Certificates
0
Other Suppliers
0

USA (Orange Book)
0

Europe

Canada
0

Australia
0

South Africa
Uploaded Dossiers
U.S. Medicaid
0
Annual Reports
0
1. 2-diphenylmethoxy-n,n-dimethylethylamine
2. Allerdryl
3. Benadryl
4. Benhydramin
5. Benylin
6. Benzhydramine
7. Citrate, Diphenhydramine
8. Dimedrol
9. Diphenhydramine Citrate
10. Diphenhydramine Citrate (1:1)
11. Diphenhydramine Hydrochloride
12. Diphenylhydramin
13. Diphenylhydramine
14. Dormin
15. Hydrochloride, Diphenhydramine
1. 58-73-1
2. Benadryl
3. Benzhydramine
4. 2-(benzhydryloxy)-n,n-dimethylethanamine
5. Alledryl
6. Probedryl
7. Dihidral
8. Antistominum
9. Benzhydraminum
10. Benzhydroamina
11. Diphantine
12. Diphenylhydramine
13. Difenhydramin
14. Allergical
15. Bagodryl
16. Baramine
17. Benachlor
18. Benadrin
19. Benodine
20. Benzantine
21. Benzhydril
22. Betramin
23. Debendrin
24. Dermistina
25. Dermodrin
26. Desentol
27. Diabenyl
28. Diabylen
29. Dibondrin
30. Difedryl
31. Drylistan
32. Histaxin
33. Hyadrine
34. Ibiodral
35. Medidryl
36. Mephadryl
37. Novamina
38. Syntedril
39. Amidryl
40. Antomin
41. Benapon
42. Benodin
43. Benylan
44. Dabylen
45. Dylamon
46. Nausen
47. Antitussive
48. Difenidramina
49. Dimedrol Base
50. Benylin
51. Difenhidramina
52. Allergina
53. Benzhydryl
54. Diphenhydraminum
55. Ethanamine, 2-(diphenylmethoxy)-n,n-dimethyl-
56. 2-(benzhydryloxy)-n,n-dimethylethylamine
57. Dibenil
58. Hydramine
59. O-benzhydryldimethylaminoethanol
60. Restamin
61. Silphen
62. Beldin
63. Diphen
64. Belix
65. Dimehydrinate
66. Far 90x2
67. 2-(diphenylmethoxy)-n,n-dimethylethanamine
68. 2-(diphenylmethoxy)-n,n-dimethylethylamine
69. Alpha-(2-dimethylaminoethoxy)diphenylmethane
70. Pm 255
71. Beta-dimethylaminoethanol Diphenylmethyl Ether
72. N-(2-(diphenylmethoxy)ethyl)-n,n-dimethylamine
73. N-(benzhydryloksy-etylo)dwumetyloamina
74. 2-benzhydryloxy-n,n-dimethylethanamine
75. [2-(diphenylmethoxy)ethyl]dimethylamine
76. Automin
77. Ethylamine, N,n-dimethyl-2-(diphenylmethoxy)-
78. Chembl657
79. 2-diphenylmethoxy-n,n-demthylethanamine
80. Beta-dimethylaminoethyl Benzhydryl Ether
81. N-[2-(benzhydryloxy)ethyl]-n,n-dimethylamine
82. 58-73-1 (free Base)
83. 8gts82s83m
84. Chebi:4636
85. Ethylamine, 2-(diphenylmethoxy)-n,n-dimethyl-
86. Dimedrolum
87. Allergan
88. Benzantin
89. Ncgc00015335-07
90. Allergeval
91. Dibendrin
92. Dimedryl
93. Dryistan
94. Rigidil
95. Syntodril
96. Aleryl
97. Ben-allergin
98. Allergan B
99. Dsstox_cid_2949
100. Difenidramina [italian]
101. Dsstox_rid_76803
102. Dsstox_gsid_22949
103. Difenhidramina [inn-spanish]
104. Diphenhydraminum [inn-latin]
105. Diphenhydramine [inn:ban:jan]
106. Cas-58-73-1
107. Beta-dimethylaminoethylbenzhydrylether
108. Restamin (tn)
109. 2-diphenylmethoxy-n,n-dimethylethylamine
110. Ccris 1959
111. Hsdb 3066
112. N-[2-(diphenylmethoxy)ethyl]-n,n-dimethylamine
113. Benadryl (hydrochloride)
114. Ncgc00015335-09
115. Cas-147-24-0
116. Einecs 200-396-7
117. N-(benzhydryloksy-etylo)dwumetyloamina [polish]
118. Beta-dimethylamino-aethyl-benzhydryl-aether [german]
119. Brn 1914136
120. Unii-8gts82s83m
121. Difenhydramine
122. Diphenhdyra
123. Dobacen
124. Beta-dimethylamino-aethyl-benzhydryl-aether
125. Allergan (salt/mix)
126. Eldadryl (salt/mix)
127. Histacyl (salt/mix)
128. Restamin (salt/mix)
129. 2-benzhydryloxy-n,n-dimethyl-ethanamine
130. Spectrum_000980
131. 2-benzhydryloxyethyl-n,n-dimethylammonium
132. Antitussive (salt/mix)
133. Prestwick0_000065
134. Prestwick1_000065
135. Prestwick2_000065
136. Prestwick3_000065
137. Spectrum2_000961
138. Spectrum3_000400
139. Spectrum4_000520
140. Spectrum5_000915
141. Lopac-d-3630
142. 2-[(diphenylmethyl)oxy]-n,n-dimethylethanamine
143. Diphenhdyra [vandf]
144. Ec 200-396-7
145. Cambridge Id 6699980
146. Schembl4064
147. Diphenhydramine [mi]
148. Lopac0_000377
149. Oprea1_254625
150. Bspbio_000249
151. Bspbio_002219
152. Dimethylamine Benzhydryl Ester
153. Diphenhydramine [inn]
154. Diphenhydramine [jan]
155. Kbiogr_001099
156. Kbioss_001460
157. 2pm
158. Mls002222276
159. Bidd:gt0152
160. Diphenhydramine (jp17/inn)
161. Diphenhydramine [hsdb]
162. Divk1c_000368
163. Orphenadrine Impurity D
164. Spbio_000961
165. Spbio_002170
166. Diphenhydramine [vandf]
167. Bpbio1_000275
168. Gtpl1224
169. Diphenhydramine [mart.]
170. 2-(benzhydryloxy)-n,n-dimethylethylamine, Hydrochloride
171. Diphenhydramine [who-dd]
172. Dtxsid4022949
173. Kbio1_000368
174. Kbio2_001460
175. Kbio2_004028
176. Kbio2_006596
177. Kbio3_001439
178. Zinc20244
179. N,n-dimethyl-2-(diphenylmethoxy)-ethylamine Hydrochloride
180. Ninds_000368
181. O-benzhydryl(dimethylamino)ethanol
182. Hms2089e06
183. Hms2230l19
184. Hms3373e03
185. Hy-b0303
186. Tox21_110127
187. Bdbm50017674
188. Mfcd00274173
189. Mfcd31699960
190. Nsc665800
191. Stk103720
192. Akos003658554
193. Tox21_110127_1
194. (2-benzhydryloxy-ethyl)-dimethyl-amine
195. Ccg-204472
196. Db01075
197. Gs-3196
198. Nsc-665800
199. Sdccgsbi-0050365.p005
200. Idi1_000368
201. Ncgc00015335-01
202. Ncgc00015335-02
203. Ncgc00015335-03
204. Ncgc00015335-04
205. Ncgc00015335-05
206. Ncgc00015335-06
207. Ncgc00015335-08
208. Ncgc00015335-10
209. Ncgc00015335-11
210. Ncgc00015335-12
211. Ncgc00015335-13
212. Ncgc00015335-14
213. Ncgc00015335-17
214. Ncgc00015335-28
215. Ncgc00024414-03
216. Ncgc00024414-04
217. Ncgc00024414-06
218. Ac-13704
219. Nci60_002916
220. Nci60_022782
221. S 51
222. Smr001307259
223. Sy246339
224. 2-(benzohydryloxy)-n,n-dimethylethylamine
225. N,n-dimethyl-2-diphenylmethyloxyethylamine
226. Sbi-0050365.p004
227. 2-(benzhydryloxy)-n,n-dimethylethanamine #
228. .beta.-(dimethylamino)ethyl Benzhydryl Ether
229. .beta.-dimethylamino-aethyl-benzhydryl-aether
230. Ab00053460
231. Cs-0013574
232. D4744
233. Ethylamine, 2-diphenylmethoxy-n,n-dimethyl-
234. Ft-0625221
235. 2-[di(phenyl)methoxy]-n,n-dimethylethanamine
236. .alpha.-(2-dimethylaminoethoxy)diphenylmethane
237. C06960
238. D00300
239. F19220
240. Ab00053460-22
241. Ab00053460-23
242. Ab00053460_24
243. Ab00053460_25
244. .beta.-(dimethylamino)ethanol Diphenylmethyl Ether
245. 274d173
246. A831996
247. Diphenhydramine; Antistominum; Benzhydramine
248. Diphenylmethanol, (n,n-dimenthylaminoethyl) Ether
249. L000227
250. Q413486
251. Q-201002
252. Brd-k47278471-003-05-7
253. Brd-k47278471-003-15-6
254. Orphenadrine Citrate Impurity D [ep Impurity]
255. 110491-04-8
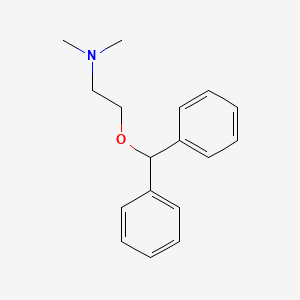
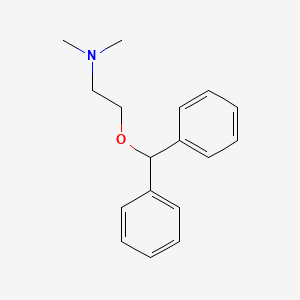
| Molecular Weight | 255.35 g/mol |
|---|---|
| Molecular Formula | C17H21NO |
| XLogP3 | 3.3 |
| Hydrogen Bond Donor Count | 0 |
| Hydrogen Bond Acceptor Count | 2 |
| Rotatable Bond Count | 6 |
| Exact Mass | 255.162314293 g/mol |
| Monoisotopic Mass | 255.162314293 g/mol |
| Topological Polar Surface Area | 12.5 Ų |
| Heavy Atom Count | 19 |
| Formal Charge | 0 |
| Complexity | 211 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 0 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
Anesthetics, Local; Anti-Allergic Agents; Antiemetics; Histamine H1 Antagonists; Hypnotics and Sedatives
National Library of Medicine's Medical Subject Headings. Diphenhydramine. Online file (MeSH, 2014). Available from, as of March 10, 2014: https://www.nlm.nih.gov/mesh/2014/mesh_browser/MBrowser.html
Antihistamines are most beneficial in the management of nasal allergies. Seasonal allergic rhinitis (e.g., hay fever) and perennial (nonseasonal) allergic rhinitis are benefited more than perennial nonallergic (vasomotor) rhinitis. Orally administered antihistamines generally provide symptomatic relief of rhinorrhea, sneezing, oronasopharyngeal irritation or itching, lacrimation, and red, irritated, or itching eyes associated with the early response to histamine. /Antihistamines; Included in US product labeling/
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 1
Antihistamines are often effective in the treatment of allergic dermatoses and other dermatoses associated with histamine release, but effectiveness varies with the causative agent and symptoms may return when the drug is stopped. /Antihistamines; Included in US product labeling/
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 1
Antihistamines may provide some benefit in certain asthmatic patients, but the drugs usually are not effective in treating bronchial asthma per se and should not be used in the treatment of severe acute asthma attacks. In addition, antihistamines are not included in the usual recommended regimens for the management of asthma, including long-term control of the disease. /Antihistamines; Included in US product labeling/
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 2
For more Therapeutic Uses (Complete) data for DIPHENHYDRAMINE (12 total), please visit the HSDB record page.
Numerous side effects ... /incl/ drowsiness, confusion, restlessness, nausea, vomiting, diarrhea, blurring of vision, diplopia, difficulty in urination, constipation, nasal stuffiness, vertigo, palpitation, headache, and insomnia. Other side effects observed were urticaria, drug rash, photosensitivity, hemolytic anemia, hypotension, epigastric distress, anaphylactic shock, tightness of the chest and wheezing, thickening of bronchial secretions, dryness of the mouth, nose and throat and tingling, and heaviness and weakness of the hands.
Troy, D.B. (Ed); Remmington The Science and Practice of Pharmacy. 21 st Edition. Lippincott Williams & Williams, Philadelphia, PA 2005, p. 1545
Like other antihistamines, diphenhydramine should be used with caution in infants and young children and should not be used in premature or full-term neonates Children younger than 6 years of age should receive diphenhydramine only under the direction of a physician. Safety and efficacy of diphenhydramine as a nighttime sleep aid in children younger than 12 years of age have not been established. In addition, children may be more prone than adults to paradoxically experience CNS stimulation rather than sedation when antihistamines are used as nighttime sleep aids. Because diphenhydramine may cause marked drowsiness that may be potentiated by other CNS depressants (e.g., sedatives, tranquilizers), the antihistamine should be used in children receiving one of these drugs only under the direction of a physician.
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 10
Prolonged use of antihistamines ... may decrease or inhibit salivary flow, thus contributing to the development of caries, periodontal disease, oral candidiasis, and discomfort. /Antihistamines/
USP Convention. USPDI - Drug Information for the Health Care Professional. 15 th ed. Volume 1. Rockville, MD: United States Pharmacopeial Convention, Inc., 1995. (Plus updates.), p. 306
Local necrosis has occurred with subcutaneous or intradermal administration of parenteral diphenhydramine.
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 10
For more Drug Warnings (Complete) data for DIPHENHYDRAMINE (18 total), please visit the HSDB record page.
...PROBABLY BEST DESCRIBED AS LYING NEAR BORDERLINE BETWEEN TOXICITY CLASSES 4 & 5. 4= VERY TOXIC: PROBABLE ORAL LETHAL DOSE (HUMAN) 50-500 MG/KG, BETWEEN 1 TEASPOON & 1 OZ FOR 70 KG PERSON (150 LB). 5= EXTREMELY TOXIC: PROBABLE ORAL LETHAL DOSE (HUMAN) 5-50 MG/KG, BETWEEN 7 DROPS & 1 TEASPOONFUL. /HYDROCHLORIDE/
Gosselin, R.E., R.P. Smith, H.C. Hodge. Clinical Toxicology of Commercial Products. 5th ed. Baltimore: Williams and Wilkins, 1984., p. II-378
Diphenhydramine is a first-generation histamine H1 receptor antagonist (H1 antihistamine) that is widely available as a non-prescription, over-the-counter (OTC) medication. As an OTC medication, diphenhydramine is typically formulated as tablets and creams indicated for use in treating sneezing, runny nose, itchy/watery eyes, itching of nose or throat, insomnia, pruritis, urticaria, insect bites/stings, allergic rashes, and nausea. Additionally, when the use of oral diphenhydramine is impractical, there are also prescription-only formulations such as diphenhydramine injection products that are effective in adults and pediatric patients (other than premature infants and neonates) for: i) the amelioration of allergic reactions to blood or plasma, in anaphylaxis as an adjunct to epinephrine and other standard measures after acute allergic reaction symptoms have been controlled, and for other uncomplicated allergic conditions of the immediate type when oral therapy is impossible or contraindicated; ii) the active treatment of motion sickness; and iii) use in parkinsonism when oral therapy is impossible or contraindicated, as follows: parkinsonism in the elderly who are unable to tolerate more potent agents; mild cases of parkinsonism in other age groups, and in other cases of parkinsonism in combination with centrally acting anticholinergic agents.
Diphenhydramine has anti-histaminic (H1-receptor), anti-emetic, anti-vertigo and sedative and hypnotic properties. The anti-histamine action occurs by blocking the spasmogenic and congestive effects of histamine by competing with histamine for H1 receptor sites on effector cells, preventing but not reversing responses mediated by histamine alone. Such receptor sites may be found in the gut, uterus, large blood vessels, bronchial muscles, and elsewhere. Anti-emetic action is by inhibition at the medullary chemoreceptor trigger zone. Anti-vertigo action is by a central antimuscarinic effect on the vestibular apparatus and the integrative vomiting center and medullary chemoreceptor trigger zone of the midbrain.
Anti-Allergic Agents
Agents that are used to treat allergic reactions. Most of these drugs act by preventing the release of inflammatory mediators or inhibiting the actions of released mediators on their target cells. (From AMA Drug Evaluations Annual, 1994, p475) (See all compounds classified as Anti-Allergic Agents.)
Histamine H1 Antagonists
Drugs that selectively bind to but do not activate histamine H1 receptors, thereby blocking the actions of endogenous histamine. Included here are the classical antihistaminics that antagonize or prevent the action of histamine mainly in immediate hypersensitivity. They act in the bronchi, capillaries, and some other smooth muscles, and are used to prevent or allay motion sickness, seasonal rhinitis, and allergic dermatitis and to induce somnolence. The effects of blocking central nervous system H1 receptors are not as well understood. (See all compounds classified as Histamine H1 Antagonists.)
Antiemetics
Drugs used to prevent NAUSEA or VOMITING. (See all compounds classified as Antiemetics.)
Sleep Aids, Pharmaceutical
Drugs used to induce SLEEP, prevent SLEEPLESSNESS, or treat SLEEP INITIATION AND MAINTENANCE DISORDERS. (See all compounds classified as Sleep Aids, Pharmaceutical.)
Anesthetics, Local
Drugs that block nerve conduction when applied locally to nerve tissue in appropriate concentrations. They act on any part of the nervous system and on every type of nerve fiber. In contact with a nerve trunk, these anesthetics can cause both sensory and motor paralysis in the innervated area. Their action is completely reversible. (From Gilman AG, et. al., Goodman and Gilman's The Pharmacological Basis of Therapeutics, 8th ed) Nearly all local anesthetics act by reducing the tendency of voltage-dependent sodium channels to activate. (See all compounds classified as Anesthetics, Local.)
Hypnotics and Sedatives
Drugs used to induce drowsiness or sleep or to reduce psychological excitement or anxiety. (See all compounds classified as Hypnotics and Sedatives.)
D04AA32
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
D - Dermatologicals
D04 - Antipruritics, incl. antihistamines, anesthetics, etc.
D04A - Antipruritics, incl. antihistamines, anesthetics, etc.
D04AA - Antihistamines for topical use
D04AA32 - Diphenhydramine
R - Respiratory system
R06 - Antihistamines for systemic use
R06A - Antihistamines for systemic use
R06AA - Aminoalkyl ethers
R06AA02 - Diphenhydramine
Absorption
Diphenhydramine is quickly absorbed after oral administration with maximum activity occurring in approximately one hour. The oral bioavailability of diphenhydramine has been documented in the range of 40% to 60%, and peak plasma concentration occurs about 2 to 3 hours after administration.
Route of Elimination
The metabolites of diphenhydramine are conjugated with glycine and glutamine and excreted in urine. Only about 1% of a single dose is excreted unchanged in urine. The medication is ultimately eliminated by the kidneys slowly, mainly as inactive metabolites.
Volume of Distribution
Diphenhydramine is widely distributed throughout the body, including the CNS. Following a 50 mg oral dose of diphenhydramine, the volume of distribution is in the range of 3.3 - 6.8 l/kg.
Clearance
Values for plasma clearance of a 50 mg oral dose of diphenhydramine has been documented as lying in the range of 600-1300 ml/min.
Distribution of diphenhydramine into human body tissues and fluids has not been fully characterized. Following IV administration in rats, highest concentrations of the drug are attained in the lungs, spleen, and brain, with lower concentrations in the heart, muscle, and liver. Following IV administration in healthy adults, diphenhydramine reportedly has an apparent volume of distribution of 188-336 L. Volume of distribution of the drug reportedly is larger in Asian (about 480 L) than white adults.
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 11
The drug crosses the placenta and has been detected in milk, although the extent of distribution into milk has not been quantitated.
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 11
Following oral administration of a single 100-mg dose in healthy adults, about 50-75% of the dose is excreted in urine within 4 days, almost completely as metabolites and with most urinary excretion occurring within the first 24-48 hours; only about 1% of a single oral dose is excreted unchanged in urine.
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 11
Diphenhydramine, given orally, reaches a maximal concentration in the blood in approximately 2 hours, remains there for another 2 hours, then falls exponentially with a plasma elimination half life of approximately 4-8 hours. The drug is distributed widely throughout the body, including the CNS. Little, if any is excreted unchanged in the urine; most appears there as metabolites.
Brunton, L. Chabner, B, Knollman, B. Goodman and Gillman's The Pharmaceutical Basis of Therapeutics, Twelth Edition, McGraw Hill Medical, New York, NY. 2011, p. 920
For more Absorption, Distribution and Excretion (Complete) data for DIPHENHYDRAMINE (7 total), please visit the HSDB record page.
Diphenhydramine undergoes rapid and extensive first-pass metabolism. In particular, two successive N-demethylations occur wherein diphenhydramine is demethylated to N-desmethyldiphenhydramine (the N-desmethyl metabolite) and then this metabolite is itself demethylated to N,N-didesmethyldiphenhydramine (the N,N-didesmethyl metabolite). Subsequently, acetyl metabolites like N-acetyl-N-desmethyldiphenhydramine are generated via the amine moiety of the N,N-didesmethyl metabolite. Additionally, the N,N-didesmethyl metabolite also undergoes some oxidation to generate the diphenylmethoxyacetic acid metabolite as well. The remaining percentage of a dose of administered diphenhydramine is excreted unchanged. The metabolites are further conjugated with glycine and glutamine and excreted in urine. Moreover, studies have determined that a variety of cytochrome P450 isoenzymes are involved in the N-demethylation that characterizes the primary metabolic pathway of diphenhydramine, including CYP2D6, CYP1A2, CYP2C9, and CYP2C19. In particular, CYP2D6 demonstrates higher affinity catalysis with the diphenhydramine substrate than the other isoenzymes identified. Consequently, inducers or inhibitors of these such CYP enzymes may potentially affect the serum concentration and incidence and/or severity of adverse effects associated with exposure to diphenhydramine.
Diphenhydramine is rapidly and apparently almost completely metabolized. Following oral administration, the drug apparently undergoes substantial first-pass metabolism in the liver. Diphenhydramine appears to be metabolized principally to diphenylmethoxyacetic acid, which may further undergo conjugation. The drug also undergoes dealkylation to form the N-demethyl and N, N-didemethyl derivatives. Diphenhydramine and its metabolites are excreted principally in urine.
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 11
Diphenhydramine is widely used as an over-the-counter antihistamine. However, the specific human cytochrome P450 (P450) isozymes that mediate the metabolism of diphenhydramine in the range of clinically relevant concentrations (0.14-0.77 microM) remain unclear. Therefore, P450 isozymes involved in N-demethylation, a main metabolic pathway of diphenhydramine, were identified by a liquid chromatography-mass spectrometry method developed in our laboratory. Among 14 recombinant P450 isozymes, CYP2D6 showed the highest activity of diphenhydramine N-demethylation (0.69 pmol/min/pmol P450) at 0.5 uM. CYP2D6 catalyzed diphenhydramine N-demethylation as a high-affinity P450 isozyme, the K(m) value of which was 1.12 +/- 0.21 uM. In addition, CYP1A2, CYP2C9, and CYP2C19 were identified as low-affinity components. In human liver microsomes, involvement of CYP2D6, CYP1A2, CYP2C9, and CYP2C19 in diphenhydramine N-demethylation was confirmed by using P450 isozyme-specific inhibitors. In addition, contributions of these P450 isozymes estimated by the relative activity factor were in good agreement with the results of inhibition studies. Although an inhibitory effect of diphenhydramine on the metabolic activity of CYP2D6 has been reported previously, the results of the present study suggest that it is not only a potent inhibitor but also a high-affinity substrate of CYP2D6. Therefore, it is worth mentioning that the sedative effect of diphenhydramine might be caused by coadministration of CYP2D6 substrate(s)/inhibitor(s). In addition, large differences in the metabolic activities of CYP2D6 and those of CYP1A2, CYP2C9, and CYP2C19 could cause the individual differences in anti-allergic efficacy and the sedative effect of diphenhydramine.
PMID:17020955 Akutsu T et al; Drug Metab Dispos 35 (1): 72-8 (2007)
Two strains of the filamentous fungus Cunninghamella elegans (ATCC 9245 and ATCC 36112) were grown in Sabouraud dextrose broth and screened for the ability to metabolize the ethanolamine-type antihistamine diphenhydramine. Based on the amount of parent drug recovered after 7 days incubation, both C. elegans strains metabolized approximately 74% of the diphenhydramine, 58% of this being identified as organic extractable metabolites. The organic extractable metabolites were isolated by reversed-phase high-performance liquid chromatography and identified by analyzing their mass and nuclear magnetic resonance spectra. Desorption chemical ionization mass spectrometry (DCIMS) with deuterated ammonia was used to differentiate possible isobaric diphenhydramine metabolites and to probe the mechanisms of ion formation under ammonia DCIMS conditions. C. elegans transformed diphenhydramine by demethylation, oxidation, and N-acetylation. The major metabolites observed were diphenhydramine-N-oxide (3%), N-desmethyldiphenhydramine (30%), N-acetyldidesmethyldiphenhydramine (13%), and N-acetyl-N-desmethyldiphenhydramine (12%). These compounds are known mammalian metabolites of diphenhydramine ... .
PMID:10772471 Moody JD et al; Appl Microbiol Biotechnol 53 (3): 310-5 (2000)
Diphenhydramine has known human metabolites that include Diphenhydramine N-glucuronide and N-Desmethyldiphenhydramine.
S73 | METXBIODB | Metabolite Reaction Database from BioTransformer | DOI:10.5281/zenodo.4056560
The elimination half-life ranges from 2.4-9.3 hours in healthy adults. The terminal elimination half-life is prolonged in liver cirrhosis.
The pharmacokinetics and pharmacodynamics of the H1-receptor antagonist diphenhydramine were studied in 21 fasting subjects divided into three age groups: elderly, (mean age 69.4 +/- 4.3 years), young adults, (mean age 31.5 +/- 10.4 years), and children, (mean age 8.9 +/- 1.7 years). All subjects ingested a single dose of diphenhydramine syrup 1.25 mg/kg. ... The mean serum elimination half-life values for diphenhydramine differed significantly in elderly adults, young adults, and children, with values of 13.5 +/- 4.2 hours, 9.2 +/- 2.5 hours, and 5.4 +/- 1.8 hours being found respectively in each age group. ...
PMID:2391399 Simons KJ et al; J Clin Pharmacol 30 (7): 665-71 (1990)
The terminal elimination half-life of diphenhydramine has not been fully elucidated, but appears to range from 2.4-9.3 hours in healthy adults. The terminal elimination half-life reportedly is prolonged in adults with liver cirrhosis.
American Society of Health-System Pharmacists 2013; Drug Information 2013. Bethesda, MD. 2013, p. 11
Diphenhydramine predominantly works via the antagonism of H1 (Histamine 1) receptors. Such H1 receptors are located on respiratory smooth muscles, vascular endothelial cells, the gastrointestinal tract (GIT), cardiac tissue, immune cells, the uterus, and the central nervous system (CNS) neurons. When the H1 receptor is stimulated in these tissues it produces a variety of actions including increased vascular permeability, promotion of vasodilation causing flushing, decreased atrioventricular (AV) node conduction time, stimulation of sensory nerves of airways producing coughing, smooth muscle contraction of bronchi and the GIT, and eosinophilic chemotaxis that promotes the allergic immune response. Ultimately, diphenhydramine functions as an inverse agonist at H1 receptors, and subsequently reverses effects of histamine on capillaries, reducing allergic reaction symptoms. Moreover, since diphenhydramine is a first-generation antihistamine, it readily crosses the blood-brain barrier and inversely agonizes the H1 CNS receptors, resulting in drowsiness, and suppressing the medullary cough center. Furthermore, H1 receptors are similar to muscarinic receptors. Consequently, diphenhydramine also acts as an antimuscarinic. It does so by behaving as a competitive antagonist of muscarinic acetylcholine receptors, resulting in its use as an antiparkinson medication. Lastly, diphenhydramine has also demonstrated activity as an intracellular sodium channel blocker, resulting in possible local anesthetic properties.
Antihistamines used in the treatment of allergy act by competing with histamine for H1-receptor sites on effector cells. They thereby prevent, but do not reverse, responses mediated by histamine alone. Antihistamines antagonize, in varying degrees, most of the pharmacological effects of histamine, including urticaria and pruritus. Also, the anticholinergic actions of most antihistamines provide a drying effect on the nasal mucosa. /Antihistamines/
USP Convention. USPDI - Drug Information for the Health Care Professional. 15 th ed. Volume 1. Rockville, MD: United States Pharmacopeial Convention, Inc., 1995. (Plus updates.), p. 304
H1 antagonists inhibit both the vasoconstrictor effects of histamine and, to a degree, the more rapid vasodilator effects mediated by activation of H1 receptors on endothelial cells (synthesis/release of NO and other mediators). /H1 Receptor Antagonists/
Brunton, L. Chabner, B, Knollman, B. Goodman and Gillman's The Pharmaceutical Basis of Therapeutics, Twelth Edition, McGraw Hill Medical, New York, NY. 2011, p. 918
H1 antagonists suppress the action of histamine on nerve endings, including the flare component of the triple response and the itching caused by intradermal injection. /H1 Receptor Antagonists/
Brunton, L. Chabner, B, Knollman, B. Goodman and Gillman's The Pharmaceutical Basis of Therapeutics, Twelth Edition, McGraw Hill Medical, New York, NY. 2011, p. 919
The first-generation antihistamines are widely prescribed medications that relieve allergic reactions and urticaria by blocking the peripheral histamine H(1) receptor. Overdose of these drugs often results in serious neuronal toxic effects, including seizures, convulsions and worsening of epileptic symptoms. The KCNQ/M K(+) channel plays a crucial role in controlling neuron excitability. Here, we demonstrate that mepyramine and diphenhydramine, two structurally related first-generation antihistamines, can act as potent KCNQ/M channel blockers. Extracellular application of these drugs quickly and reversibly reduced KCNQ2/Q3 currents heterologously expressed in HEK293 cells. The current inhibition was concentration and voltage dependent. The estimated IC(50) (12.5 and 48.1 microM, respectively) is within the range of drug concentrations detected in poisoned patients (30-300 microM). Both drugs shifted the I-V curve of KCNQ2/Q3 channel to more depolarized potentials and altered channel gating properties by prolonging activation and shortening deactivation kinetics. Mepyramine also inhibited the individual homomeric KCNQ1-4 and heteromeric KCNQ3/Q5 currents. Moreover, mepyramine inhibited KCNQ2/Q3 current in an outside-out patch excised from HEK293 cells and the inhibitory effect was neither observed when it was applied intracellularly nor affected by blocking phospholipase C (PLC) activity, indicating an extracellular and direct channel blocking mechanism. Finally, in cultured rat superior cervical ganglion (SCG) neurons, mepyramine reduced the M type K(+) current in a concentration-dependent manner and led to marked membrane potential depolarization. It is likely that these effects may be involved in the adverse neuroexcitatory effects observed in patients experiencing an overdose of antihistamines.
PMID:18222495 Liu B et al; Neuropharmacology 54 (4): 629-39 (2008)
The first generation antihistamines, such as diphenhydramine, are fairly potent muscarinic antagonists in addition to being H1 selective antihistamines. The antimuscarinic action is often not desirable since it is in part responsible for the drying of secretions in the airways and the sedative effect. We therefore examined a number of antihistamines for antimuscarinic effects on ion transport by mucus gland cells isolated from the airways of swine. Enzymatically isolated airway mucus gland cells were purified utilizing density gradients and grown in culture on porous inserts (Millicell HA) at an air interface. Cells grown in this manner maintain phenotype and polarity. Transport of ions, as short-circuit current measured under voltage-clamp, was measured in response to acetylcholine (ACh) or histamine applied to the serosal side of the gland cell layers. Concentration-response relationships for ACh or histamine were generated in the presence and absence of various drugs. The potencies against muscarinic receptor activation were estimated using the dose-ratio method of Schild. Three known muscarinic antagonists were used to validate the system. Atropine had a pA2 of 9.4 +/- 0.1 (n = 9). 4-DAMP and methoctramine had pA2 values of 8.6 +/- 0.1 and 5.6 +/- 0.1, respectively (n = 12, 11) all consistent with inhibition of an M3 subtype muscarinic receptor. The rank order of potency of the antihistamines against the inhibition of M3 receptors was desloratadine = diphenhydramine > hydroxyzine (pA2; 6.4, 6.2, 4.8, respectively). pA2 values for fexofenadine, loratadine and cetirizine were not determined since they had no effect on the cholinergic response at the highest drug concentrations tested (10, 10 and 100 microM, respectively). The pA2 values for the antihistamines against the histamine response could not be calculated, but the estimates of the rank order of potency were estimated to be desloratadine > cetirizine approximate to hydroxyzine > fexofenadine > loratadine > diphenhydramine. The rank order of selectivity for histamine receptors over muscarinic receptors was estimated to be cetirizine approximate to fexofenadine > loratadine > desloratadine > or = hydroxyzine > or = diphenhydramine.
PMID:15790419 Full text: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1079883 Liu H, Farley JM; BMC Pharmacol 5: 8 (2005)






