


API Suppliers

US DMFs Filed

CEP/COS Certifications

JDMFs Filed
Other Certificates
Other Suppliers
0

USA (Orange Book)

Europe

Canada

Australia

South Africa
Uploaded Dossiers
U.S. Medicaid
Annual Reports
0
1. Boehringer, Digoxina
2. Digacin
3. Digitek
4. Digoregen
5. Digoxina Boehringer
6. Digoxine Nativelle
7. Dilanacin
8. Hemigoxine Nativelle
9. Lanacordin
10. Lanicor
11. Lanoxicaps
12. Lanoxin
13. Lanoxin Pg
14. Lanoxin-pg
15. Lenoxin
16. Mapluxin
17. Nativelle, Digoxine
18. Nativelle, Hemigoxine
1. 20830-75-5
2. Lanoxin
3. 12beta-hydroxydigitoxin
4. Digacin
5. Dilanacin
6. Rougoxin
7. Lanoxicaps
8. Mapluxin
9. Dynamos
10. Vanoxin
11. Davoxin
12. Digosin
13. Fargoxin
14. Natigoxin
15. Lanocardin
16. Cordioxil
17. Digoxinum
18. Toloxin
19. Stillacor-
20. Digoxin Pediatric
21. Chebi:4551
22. Mls000069819
23. Cardiogoxin
24. Lanacordin
25. Eudigox
26. Lanacrist
27. Lenoxin
28. Smr000059217
29. Neo-lanicor
30. (3beta,5beta,12beta)-3-{[2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-beta-d-ribo-hexopyranosyl]oxy}-12,14-dihydroxycard-20(22)-enolide
31. Digoxin Nativelle
32. Lanoxin Pg
33. Sk-digoxin
34. Homolle's Digitalin
35. Nsc 95100
36. Nsc-95100
37. Ncgc00090797-03
38. 73k4184t59
39. Dsstox_cid_2934
40. Digoxin, Analytical Standard
41. Dsstox_rid_76794
42. Coragoxine
43. Dsstox_gsid_22934
44. Lenoxicaps
45. Neodioxanin
46. Cardigox
47. Cardioxin
48. Digomal
49. Lanikor
50. Lanorale
51. Purgoxin
52. 3-[(3s,5r,8r,9s,10s,12r,13s,14s,17r)-3-[(2r,4s,5s,6r)-5-[(2s,4s,5s,6r)-5-[(2s,4s,5s,6r)-4,5-dihydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyloxan-2-yl]oxy-12,14-dihydroxy-10,13-dimethyl-1,2,3,4,5,6,7,8,9,11,12,15,16,17-tetradecahydrocyclopenta[a]phenanthren-17-yl]-2h-furan-5-one
53. Dixina
54. Grexin
55. Digon
56. Dokim
57. Digitek
58. Digoxine
59. Chloroformic Digitalin
60. Lanoxicaps (tn)
61. [3h]digoxin
62. 4-[(1s,2s,5s,7r,10r,11s,14r,15s,16r)-5-{[(2r,4s,5s,6r)-5-{[(2s,4s,5s,6r)-5-{[(2s,4s,5s,6r)-4,5-dihydroxy-6-methyloxan-2-yl]oxy}-4-hydroxy-6-methyloxan-2-yl]oxy}-4-hydroxy-6-methyloxan-2-yl]oxy}-11,16-dihydroxy-2,15-dimethyltetracyclo[8.7.0.0^{2,7}.0^{11,15}]heptadecan-14-yl]-2,5-dihydrofuran-2-one
63. Smr000653537
64. Hemigoxine Nativelle
65. Lanoxin (tn)
66. [3h]-digoxin
67. Acygoxin
68. Digoksyna
69. Digonix
70. Digossina
71. Digoxina
72. Dimecip
73. Lifusin
74. Saroxin
75. Digos
76. Digoxin-sandoz
77. Digoxina-sandoz
78. Digoxin-zori
79. Digoxine Navtivelle
80. Novodigal [inj.]
81. 3-[(3s,5r,8r,9s,10s,12r,13s,14s,17r)-3-[(2r,4s,5s,6r)-5-[(2s,4s,5s,6r)-5-[(2s,4s,5s,6r)-4,5-dihydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyloxan-2-yl]oxy-12,14-dihydr
82. Oxy-10,13-dimethyl-1,2,3,4,5,6,7,8,9,11,12,15,16,17-tetradecahydrocyclopenta[a]phenanthren-17-yl]-2h-furan-5-one
83. Prestwick_170
84. Digoksyna [polish]
85. Digossina [dcit]
86. Cas-20830-75-5
87. Mfcd00003674
88. 12a-hydroxydigitoxin
89. 3b0w
90. Lanoxin Pediatric
91. Digoxin [vandf]
92. Digoxinum [inn-latin]
93. 12bet.-hydroxydigitoxin
94. Digoxin [hsdb]
95. Digoxin [iarc]
96. Digoxin [inn]
97. Digoxin [jan]
98. Digoxigenin-tridigitoxosid
99. Digoxin [mi]
100. Digoxina [inn-spanish]
101. Digoxin [mart.]
102. Opera_id_1134
103. Prestwick0_000437
104. Prestwick1_000437
105. Prestwick2_000437
106. Prestwick3_000437
107. Digoxin (jp17/usp)
108. Digoxin [usp-rs]
109. Digoxin [who-dd]
110. Digoxin [who-ip]
111. 12 Beta -hydroxydigitoxin
112. Epitope Id:122964
113. Chembl1751
114. Bidd:pxr0148
115. Schembl20506
116. Bspbio_000454
117. Mls001055371
118. Mls001076495
119. Digoxin [orange Book]
120. Digoxin For Peak Identification
121. Spbio_002393
122. Digoxin [ep Monograph]
123. Bpbio1_000500
124. Gtpl4725
125. Gtpl4726
126. Hsdb 214
127. Digoxin [usp Monograph]
128. Digoxin [usp:inn:ban:jan]
129. Digoxin 1.0 Mg/ml In Methanol
130. Dtxsid5022934
131. Bdbm46355
132. Cid_2724385
133. Digoxinum [who-ip Latin]
134. Regid_for_cid_2724385
135. Hms1569g16
136. Hms2096g16
137. Hms2232g20
138. Hms3713g16
139. Unii-73k4184t59
140. Digoxigenin-tridigitoxosid [german]
141. Hy-b1049
142. Einecs 244-068-1
143. Tox21_111025
144. Tox21_201678
145. Tox21_303050
146. 20830-75-5 (free)
147. S4290
148. Akos015895113
149. Akos024283494
150. Zinc242548690
151. Ccg-220437
152. Cs-4571
153. Db00390
154. Brn 0077011
155. Ncgc00090797-01
156. Ncgc00090797-02
157. Ncgc00090797-04
158. Ncgc00090797-05
159. Ncgc00090797-06
160. Ncgc00090797-07
161. Ncgc00090797-09
162. Ncgc00090797-12
163. Ncgc00090797-15
164. Ncgc00257022-01
165. Ncgc00259227-01
166. As-13281
167. Card-20(22)-enolide, 3-((o-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1-4)-o-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1-4)-2,6-dideoxy-beta-d-ribo-hexopyranosyl)oxy)-12,14-dihydroxy-, (3beta,5beta,12beta)-
168. B7684
169. D1828
170. C06956
171. D00298
172. 5-18-04-00381 (beilstein Handbook Reference)
173. 830d755
174. A814956
175. Q422222
176. Sr-01000721866
177. Digoxin, Certified Reference Material, Tracecert(r)
178. J-013666
179. Sr-01000721866-3
180. Sr-01000721866-4
181. Brd-k23478508-001-03-7
182. Digoxin, European Pharmacopoeia (ep) Reference Standard
183. 0b9662a7-264e-4acd-94b2-9e1138c0ca5a
184. Digoxin, United States Pharmacopeia (usp) Reference Standard
185. Digoxin, Pharmaceutical Secondary Standard; Certified Reference Material
186. 3beta,12beta,14-trihydroxy-5beta,14beta-card-20(22)-enolid-3-tridigitoxosid
187. Digoxin For Peak Identification, European Pharmacopoeia (ep) Reference Standard
188. Digoxin Solution, 1.0 Mg/ml In Methanol, Ampule Of 1 Ml, Certified Reference Material
189. (3beta,5beta,12beta)-3-((o-2,6-dideoxy-beta-d-ribo-hexapyranosyl-(1-4)-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1-4)-2,6-dideoxy-beta-d-ribo-hexopyranosyl)oxy)-12,14-dihydroxycard-20(22)-enolide
190. 3-[(3s,5r,10s,12r,13s,14s,17r)-3-[(2r,4s,5s,6r)-5-[(2s,4s,5s,6r)-5-[(2s,4s,5s,6r)-4,5-dihydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyloxan-2-yl]oxy-12,14-dihydroxy-10,13-dimethyl-1,2,3,4,5,6,7,8,9,11,12,15,16,17-tetradecahydrocyclopenta[a]phenanthren-17-yl]-2h-furan-5-one
191. 3-[(3s,5r,8r,9s,10s,12r,13s,14s,17r)-10,13-dimethyl-3-[(2r,4s,5s,6r)-6-methyl-5-[(2s,4s,5s,6r)-6-methyl-5-[(2s,4s,5s,6r)-6-methyl-4,5-bis(oxidanyl)oxan-2-yl]oxy-4-oxidanyl-oxan-2-yl]oxy-4-oxidanyl-oxan-2-yl]oxy-12,14-bis(oxidanyl)-1,2,3,4,5,6,7,8,9,11,12,
192. 3-[(3s,5r,8r,9s,10s,12r,13s,14s,17r)-3-[(2r,4s,5s,6r)-5-[(2s,4s,5s,6r)-5-[(2s,4s,5s,6r)-4,5-dihydroxy-6-methyl-tetrahydropyran-2-yl]oxy-4-hydroxy-6-methyl-tetrahydropyran-2-yl]oxy-4-hydroxy-6-methyl-tetrahydropyran-2-yl]oxy-12,14-dihydroxy-10,13-dimethyl-1,2,3,4,5,6,7,8,9,11,12,15,16,17-tetradecahydrocyclopenta[a]phenanthren-17-yl]-2h-furan-5-one
193. 3-[(3s,5r,8r,9s,10s,12r,13s,14s,17r)-3-[(2r,4s,5s,6r)-5-[(2s,4s,5s,6r)-5-[(2s,4s,5s,6r)-4,5-dihydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyloxan-2-yl]oxy-12,14-dihydroxy-10,13-dimethyl-1,2,3,4,5,6,7,8,9,11,12,15,16,17-tet
194. 3-[(3s,5r,8r,9s,10s,12r,13s,14s,17r)-3-[[(2r,4s,5s,6r)-5-[[(2s,4s,5s,6r)-5-[[(2s,4s,5s,6r)-4,5-dihydroxy-6-methyl-2-oxanyl]oxy]-4-hydroxy-6-methyl-2-oxanyl]oxy]-4-hydroxy-6-methyl-2-oxanyl]oxy]-12,14-dihydroxy-10,13-dimethyl-1,2,3,4,5,6,7,8,9,11,12,15,16,
195. 3.beta.-((o-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl-(1->4)-o-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl)oxy)-12.beta.,14-dihydroxy-5.beta.-card-20(22)-enolide
196. 3beta-((o-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1-4)-o-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1-4)-2,6-dideoxy-beta-d-ribo-hexopyranosyl)oxy)-12beta,14-dihydroxy-5beta-card-20(22)-enolide
197. 4-((1s,2s,5s,11s,15s,7r,10r,14r,16r)-5-{5-[5-((2s,4s,5s,6r)-4,5-dihydroxy-6-me Thyl(2h-3,4,5,6-tetrahydropyran-2-yloxy))(4s,5s,2r,6r)-4-hydroxy-6-methyl(2h-3 ,4,5,6-tetrahydropyran-2-yloxy)](4s,5s,2r,6r)-4-hydroxy-6-methyl(2h-3,4,5,6-te Trahydropyran-2-yl
198. 4-((3s,5r,8r,9s,10s,12r,13s,14s,17r)-3-(((2r,4s,5s,6r)-5-(((2s,4s,5s,6r)-5-(((2s,4s,5s,6r)-4,5-dihydroxy-6-methyltetrahydro-2h-pyran-2-yl)oxy)-4-hydroxy-6-methyltetrahydro-2h-pyran-2-yl)oxy)-4-hydroxy-6-methyltetrahydro-2h-pyran-2-yl)oxy)-12,14-dihydroxy-10,13-dimethylhexadecahydro-1h-cyclopenta[a]phenanthren-17-yl)furan-2(5h)-one
199. 4-[(3s,5r,8r,9s,10s,12r,13s,14s)-3-[(2s,4s,5r,6r)-5-[(2s,4s,5r,6r)-5-[(2s,4s,5r,6r)-4,5-dihydroxy-6-methyloxan-2-yl]oxy-4-hydroxy-6-methyl-oxan-2-yl]oxy-4-hydroxy-6-methyl-oxan-2-yl]oxy-12,14-dihydroxy-10,13-dimethyl-1,2,3,4,5,6,7,8,9,11,12,15,16,17-tetradecahydrocyclopenta[a]phenanthren-17-yl]-5h-furan-2-one
200. Card-20(22)-enolide, 3-((o-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl-(1->4)-o-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl)oxy)-12,14-dihydroxy-,(3.beta.,5.beta.,12.beta.)-
201. Card-20(22)-enolide, 3-((o-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1->4)-o-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1->4)-2,6-dideoxy-beta-d-ribo-hexopyranosyl)oxy)-12,14-dihydroxy-, (3beta,5beta,12beta)-
202. Card-20(22)-enolide, 3-((o-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1.fwdarw.4)-o-2,6-dideoxy-beta-d-ribo-hexopyranosyl-(1.fwdarw.4)-2,6-dideoxy-beta-d-ribo-hexopyranosyl)oxy)-12,14-dihydroxy-, (3beta,5beta,12beta)-
203. Card-20(22)-enolide, 3-[[o-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl-(1-->4)-o-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl-(1-->4)-2,6-dideoxy-.beta.-d-ribo-hexopyranosyl]oxy]-12,14-dihydroxy-, (3.beta.,5.beta.,12.beta.)-
1. Lanitop
2. Methyldigoxin
3. Medigoxin
4. Metildigoxin
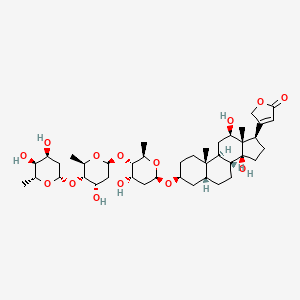
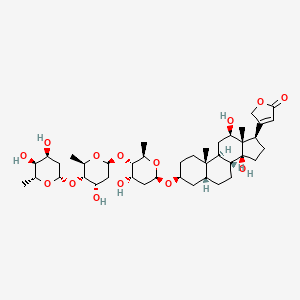
| Molecular Weight | 780.9 g/mol |
|---|---|
| Molecular Formula | C41H64O14 |
| XLogP3 | 1.3 |
| Hydrogen Bond Donor Count | 6 |
| Hydrogen Bond Acceptor Count | 14 |
| Rotatable Bond Count | 7 |
| Exact Mass | 780.42960671 g/mol |
| Monoisotopic Mass | 780.42960671 g/mol |
| Topological Polar Surface Area | 203 Ų |
| Heavy Atom Count | 55 |
| Formal Charge | 0 |
| Complexity | 1450 |
| Isotope Atom Count | 0 |
| Defined Atom Stereocenter Count | 21 |
| Undefined Atom Stereocenter Count | 0 |
| Defined Bond Stereocenter Count | 0 |
| Undefined Bond Stereocenter Count | 0 |
| Covalently Bonded Unit Count | 1 |
| 1 of 4 | |
|---|---|
| Drug Name | Digoxin |
| PubMed Health | Digoxin |
| Drug Classes | Antiarrhythmic, Cardiovascular Agent |
| Drug Label | Digoxin Tablets, USP are one of the cardiac (or digitalis) glycosides, a closely related group of drugs having in common specific effects on the myocardium. These drugs are found in a number of plants. Digoxin is extracted from the leaves of Digitali... |
| Active Ingredient | Digoxin |
| Dosage Form | Elixir; Injectable; Tablet |
| Route | Injection; Oral |
| Strength | 0.05mg/ml; 0.25mg; 0.25mg/ml; 0.125mg |
| Market Status | Prescription |
| Company | Hikma Maple; Stevens J; Sandoz; Hikma Pharms; Impax Labs; Roxane |
| 2 of 4 | |
|---|---|
| Drug Name | Lanoxin |
| PubMed Health | Digoxin |
| Drug Classes | Antiarrhythmic, Cardiovascular Agent |
| Drug Label | LANOXIN (digoxin) is one of the cardiac (or digitalis) glycosides, a closely related group of drugs having in common specific effects on the myocardium.These drugs are found in a number of plants. Digoxin is extracted from the leaves of Digitalis l... |
| Active Ingredient | Digoxin |
| Dosage Form | Tablet; Injectable |
| Route | Injection; Oral |
| Strength | 0.0625mg; 0.25mg; 0.25mg/ml; 0.1875mg; 0.125mg |
| Market Status | Prescription |
| Company | Covis Injectables; Covis Pharma |
| 3 of 4 | |
|---|---|
| Drug Name | Digoxin |
| PubMed Health | Digoxin |
| Drug Classes | Antiarrhythmic, Cardiovascular Agent |
| Drug Label | Digoxin Tablets, USP are one of the cardiac (or digitalis) glycosides, a closely related group of drugs having in common specific effects on the myocardium. These drugs are found in a number of plants. Digoxin is extracted from the leaves of Digitali... |
| Active Ingredient | Digoxin |
| Dosage Form | Elixir; Injectable; Tablet |
| Route | Injection; Oral |
| Strength | 0.05mg/ml; 0.25mg; 0.25mg/ml; 0.125mg |
| Market Status | Prescription |
| Company | Hikma Maple; Stevens J; Sandoz; Hikma Pharms; Impax Labs; Roxane |
| 4 of 4 | |
|---|---|
| Drug Name | Lanoxin |
| PubMed Health | Digoxin |
| Drug Classes | Antiarrhythmic, Cardiovascular Agent |
| Drug Label | LANOXIN (digoxin) is one of the cardiac (or digitalis) glycosides, a closely related group of drugs having in common specific effects on the myocardium.These drugs are found in a number of plants. Digoxin is extracted from the leaves of Digitalis l... |
| Active Ingredient | Digoxin |
| Dosage Form | Tablet; Injectable |
| Route | Injection; Oral |
| Strength | 0.0625mg; 0.25mg; 0.25mg/ml; 0.1875mg; 0.125mg |
| Market Status | Prescription |
| Company | Covis Injectables; Covis Pharma |
Anti-Arrhythmia Agents; Cardiotonic Agents; Enzyme Inhibitors
National Library of Medicine's Medical Subject Headings. Digoxin. Online file (MeSH, 2018). Available from, as of August 29, 2018: https://meshb.nlm.nih.gov/search
/CLINICAL TRIALS/ ClinicalTrials.gov is a registry and results database of publicly and privately supported clinical studies of human participants conducted around the world. The Web site is maintained by the National Library of Medicine (NLM) and the National Institutes of Health (NIH). Each ClinicalTrials.gov record presents summary information about a study protocol and includes the following: Disease or condition; Intervention (for example, the medical product, behavior, or procedure being studied); Title, description, and design of the study; Requirements for participation (eligibility criteria); Locations where the study is being conducted; Contact information for the study locations; and Links to relevant information on other health Web sites, such as NLM's MedlinePlus for patient health information and PubMed for citations and abstracts for scholarly articles in the field of medicine. Digoxin is included in the database.
NIH/NLM; ClinicalTrials.Gov. Available from, as of August 29, 2018: https://clinicaltrials.gov/
Digoxin tablets, USP are indicated for the treatment of mild to moderate heart failure in adults. Digoxin tablets, USP increase left ventricular ejection fraction and improve heart failure symptoms as evidenced by improved exercise capacity and decreased heart failure-related hospitalizations and emergency care, while having no effect on mortality. Where possible, digoxin tablets, USP should be used in combination with a diuretic and an angiotensin-converting enzyme (ACE) inhibitor. /Included in US product label/
NIH; DailyMed. Current Medication Information for Digoxin Tablet (Updated: February 29, 2016). Available from, as of September 4, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=dfac7f13-28be-423d-9389-9089da29da17
Digoxin tablets, USP increase myocardial contractility in pediatric patients with heart failure. /Included in US product label/
NIH; DailyMed. Current Medication Information for Digoxin Tablet (Updated: February 29, 2016). Available from, as of September 4, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=dfac7f13-28be-423d-9389-9089da29da17
For more Therapeutic Uses (Complete) data for Digoxin (16 total), please visit the HSDB record page.
Patients with Wolff-Parkinson-White syndrome who develop atrial fibrillation are at high risk of ventricular fibrillation. Treatment of these patients with digoxin leads to greater slowing of conduction in the atrioventricular node than in accessory pathways, and the risks of rapid ventricular response leading to ventricular fibrillation are thereby increased.
NIH; DailyMed. Current Medication Information for Digoxin Tablet (Updated: February 29, 2016). Available from, as of September 4, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=dfac7f13-28be-423d-9389-9089da29da17
Cardiac glycosides should be used with caution in patients with severe pulmonary disease, hypoxia, myxedema, acute myocardial infarction, severe heart failure, acute myocarditis (including rheumatic carditis) or an otherwise damaged myocardium, since the likelihood of cardiac glycoside-induced arrhythmias is increased in these patients. The possibility that use of cardiac glycosides in some patients with acute myocardial infarction may result in an undesirable increase in oxygen demand and associated ischemia should be considered. In patients with rheumatic carditis, dosage should be low initially and increased gradually until a beneficial effect is obtained or, if improvement does not occur in these patients, the drug should be discontinued. Cardiac glycosides should be used with caution in patients with chronic constrictive pericarditis since these patients may respond unfavorably. Cardiac glycosides should be administered with extreme caution in patients with acute glomerulonephritis and heart failure; if the drugs are necessary, total daily dosage must be reduced and given in divided doses with constant ECG monitoring. These patients should be treated concomitantly with diuretics and hypotensive agents and the glycoside should be discontinued as soon as possible. Cardiac glycosides also should be used with extreme caution, if at all, in patients with idiopathic hypertrophic subaortic stenosis because increased obstruction to left ventricular outflow may result. Patients with certain disorders involving heart failure associated with preserved left ventricular ejection fraction (e.g., restrictive cardiomyopathy, constrictive pericarditis, amyloid heart disease, acute cor pulmonale) may be particularly susceptible to the toxicity of cardiac glycosides. /Cardiac glycosides/
American Society of Health-System Pharmacists; Drug Information 2018. Bethesda, MD. 2018, p. 1814
Signs and symptoms of digoxin toxicity include anorexia, nausea, vomiting, visual changes and cardiac arrhythmias (first-degree, second-degree (Wenckebach), or third-degree heart block (including asystole); atrial tachycardia with block; AV dissociation; accelerated junctional (nodal) rhythm; unifocal or multiform ventricular premature contractions (especially bigeminy or trigeminy); ventricular tachycardia; and ventricular fibrillation). Toxicity is usually associated with digoxin levels greater than 2 ng/mL although symptoms may also occur at lower levels. Low body weight, advanced age or impaired renal function, hypokalemia, hypercalcemia, or hypomagnesemia may predispose to digoxin toxicity. Obtain serum digoxin levels in patients with signs or symptoms of digoxin therapy and interrupt or adjust dose if necessary. Assess serum electrolytes and renal function periodically.
NIH; DailyMed. Current Medication Information for Digoxin Tablet (Updated: February 29, 2016). Available from, as of September 4, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=dfac7f13-28be-423d-9389-9089da29da17
The earliest and most frequent manifestation of digoxin toxicity in infants and children is the appearance of cardiac arrhythmias, including sinus bradycardia. In children, the use of digoxin may produce any arrhythmia. The most common are conduction disturbances or supraventricular tachyarrhythmias, such as atrial tachycardia (with or without block) and junctional (nodal) tachycardia. Ventricular arrhythmias are less common. Sinus bradycardia may be a sign of impending digoxin intoxication, especially in infants, even in the absence of first-degree heart block. Any arrhythmias or alteration in cardiac conduction that develops in a child taking digoxin should initially be assumed to be a consequence of digoxin intoxication.
NIH; DailyMed. Current Medication Information for Digoxin Tablet (Updated: February 29, 2016). Available from, as of September 4, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=dfac7f13-28be-423d-9389-9089da29da17
For more Drug Warnings (Complete) data for Digoxin (33 total), please visit the HSDB record page.
Estimated single lethal dose is 10-20 mg.
Gosselin, R.E., R.P. Smith, H.C. Hodge. Clinical Toxicology of Commercial Products. 5th ed. Baltimore: Williams and Wilkins, 1984., p. III-153
Digoxin is indicated in the following conditions: 1) For the treatment of mild to moderate heart failure in adult patients. 2) To increase myocardial contraction in children diagnosed with heart failure. 3) To maintain control ventricular rate in adult patients diagnosed with chronic atrial fibrillation. In adults with heart failure, when it is clinically possible, digoxin should be administered in conjunction with a diuretic and an angiotensin-converting enzyme (ACE) inhibitor for optimum effects.
Digoxin is a positive inotropic and negative chronotropic drug, meaning that it increases the force of the heartbeat and decreases the heart rate. The decrease in heart rate is particularly useful in cases of atrial fibrillation, a condition characterized by a fast and irregular heartbeat. The relief of heart failure symptoms during digoxin therapy has been demonstrated in clinical studies by increased exercise capacity and reduced hospitalization due to heart failure and reduced heart failure-related emergency medical visits. Digoxin has a narrow therapeutic window. **A note on cardiovascular risk** Digoxin poses a risk of rapid ventricular response that can cause ventricular fibrillation in patients with an accessory atrioventricular (AV) pathway. Cardiac arrest as a result of ventricular fibrillation is fatal. An increased risk of fatal severe or complete heart block is present in individuals with pre-existing sinus node disease and AV block who take digoxin.
Anti-Arrhythmia Agents
Agents used for the treatment or prevention of cardiac arrhythmias. They may affect the polarization-repolarization phase of the action potential, its excitability or refractoriness, or impulse conduction or membrane responsiveness within cardiac fibers. Anti-arrhythmia agents are often classed into four main groups according to their mechanism of action: sodium channel blockade, beta-adrenergic blockade, repolarization prolongation, or calcium channel blockade. (See all compounds classified as Anti-Arrhythmia Agents.)
Cardiotonic Agents
Agents that have a strengthening effect on the heart or that can increase cardiac output. They may be CARDIAC GLYCOSIDES; SYMPATHOMIMETICS; or other drugs. They are used after MYOCARDIAL INFARCT; CARDIAC SURGICAL PROCEDURES; in SHOCK; or in congestive heart failure (HEART FAILURE). (See all compounds classified as Cardiotonic Agents.)
Enzyme Inhibitors
Compounds or agents that combine with an enzyme in such a manner as to prevent the normal substrate-enzyme combination and the catalytic reaction. (See all compounds classified as Enzyme Inhibitors.)
C01AA05
S76 | LUXPHARMA | Pharmaceuticals Marketed in Luxembourg | Pharmaceuticals marketed in Luxembourg, as published by d'Gesondheetskeess (CNS, la caisse nationale de sante, www.cns.lu), mapped by name to structures using CompTox by R. Singh et al. (in prep.). List downloaded from https://cns.public.lu/en/legislations/textes-coordonnes/liste-med-comm.html. Dataset DOI:10.5281/zenodo.4587355
C - Cardiovascular system
C01 - Cardiac therapy
C01A - Cardiac glycosides
C01AA - Digitalis glycosides
C01AA05 - Digoxin
Absorption
Digoxin is approximately 70-80% absorbed in the first part of the small bowel. The bioavailability of an oral dose varies from 50-90%, however, oral gelatinized capsules of digoxin are reported to have a bioavailability of 100%. Tmax, or the time to reach the maximum concentration of digoxin was measured to be 1.0 h in one clinical study of healthy patients taking 0.25 mg of digoxin with a placebo. Cmax, or maximum concentration, was 1.32 0.18 ng/ml1 in the same study, and AUC (area under the curve) was 12.5 2.38 ng/ml1. If digoxin is ingested after a meal, absorption is slowed but this does not change the total amount of absorbed drug. If digoxin is taken with meals that are in fiber, absorption may be decreased. **A note on gut bacteria** An oral dose of digoxin may be transformed into pharmacologically inactive products by bacteria in the colon. Studies have indicated that 10% of patients receiving digoxin tablets will experience the degradation of at least 40% of an ingested dose of digoxin by gut bacteria. Several antibiotics may increase the absorption of digoxin in these patients, due to the elimination of gut bacteria, which normally cause digoxin degradation. **A note on malabsorption** Patients with malabsorption due to a variety of causes may have a decreased ability to absorb digoxin. P-glycoprotein, located on cells in the intestine, may interfere with digoxin pharmacokinetics, as it is a substrate of this efflux transporter. P-glycoprotein can be induced by other drugs, therefore reducing the effects of digoxin by increasing its efflux in the intestine.
Route of Elimination
The elimination of digoxin is proportional to the total dose, following first order kinetics. After intravenous (IV) administration to healthy subjects, 50-70% of the dose is measured excreted as unchanged digoxin in the urine. Approximately 25 to 28% of digoxin is eliminated outside of the kidney. Biliary excretion appears to be of much less importance than renal excretion. Digoxin is not effectively removed from the body by dialysis, exchange transfusion, or during cardiopulmonary bypass because most of the drug is bound to extravascular tissues.
Volume of Distribution
This drug is widely distributed in the body, and is known to cross the blood-brain barrier and the placenta. The apparent volume of distribution of digoxin is 475-500 L. A large portion of digoxin is distributed in the skeletal muscle followed by the heart and kidneys. It is important to note that the elderly population, generally having a decreased muscle mass, may show a lower volume of digoxin distribution.
Clearance
The clearance of digoxin closely correlates to creatinine clearance, and does not depend on urinary flow. Individuals with renal impairment or failure may exhibit extensively prolonged half-lives. It is therefore important to titrate the dose accordingly and regularly monitor serum digoxin levels. One pharmacokinetic study measured the mean body clearance of intravenous digoxin to be 88 44ml/min/l.73 m. Another study provided mean clearance values of 53 ml/min/1.73 m in men aged 73-81 and 83 ml/min/1.73 m in men aged 20-33 years old after an intravenous digoxin dose.
/MILK/ Maximum milk concentrations of 0.96 and 0.61 ng/mL observed at 4-6 hrs after administering single dose of 0.25 mg to 2 women. Maternal plasma concentration slightly higher than concentration in milk.
Loughnan PM; J Pediatr (St Louis) 92 (6): 1019-20 (1978)
/MILK/ Digoxin is excreted into breast milk. ... Digoxin milk/plasma ratios have varied from 0.6 to 0.9. Although these amounts seem high, they represent very small amounts of digoxin due to significant maternal protein binding.
Briggs, G.G., Freeman, R.K., Yaffee, S.J.; Drugs in Pregancy and Lactation Tenth Edition. Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia, PA. 2015, p. 406
Following oral administration, peak serum concentrations of digoxin occur at 1 to 3 hours. Absorption of digoxin from digoxin tablets has been demonstrated to be 60 to 80% complete compared to an identical intravenous dose of digoxin (absolute bioavailability). When digoxin tablets are taken after meals, the rate of absorption is slowed, but the total amount of digoxin absorbed is usually unchanged. When taken with meals high in bran fiber, however, the amount absorbed from an oral dose may be reduced.
NIH; DailyMed. Current Medication Information for Digoxin Tablet (Updated: February 29, 2016). Available from, as of September 4, 2018: https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=dfac7f13-28be-423d-9389-9089da29da17
/MILK/ In order to find out whether digoxin therapy of nursing mothers might produce discomfort in suckling infants we have investigated the kinetics of the transfer of digoxin from plasma to milk in 11 nursing mothers. After intravenous or oral application of a single dose of 0.5 mg or 0.75 mg digoxin simultaneous serum, fore- and hindmilk samples were taken. Obviously, a rapid equilibrium occurred between the serum and the milk compartments and there was no difference between fore- and hindmilk. All three digoxin concentration profiles ran parallel with a milk to serum ratio of 0.6 to 0.7. The curves could best be fitted by the sum of two exponential functions. For predicting the digoxin intake into the suckling infant, simulations were carried out on the basis of two coupled compartment models. When the kinetic milk data as well as the kinetic data obtained in infants were fitted by this model it could be shown that even in the case of long half-lives only about 3% of the therapeutic drug levels were reached in the baby. Thus, one can conclude that digoxin accumulation to toxic concentrations should not occur in infants of women treated with appropriate doses of digoxin.
PMID:7075628 Reinhardt D et al; Eur J Pediatr 138 (1): 49-52 (1982)
For more Absorption, Distribution and Excretion (Complete) data for Digoxin (19 total), please visit the HSDB record page.
About 13% of a digoxin dose is found to be metabolized in healthy subjects. Several urinary metabolites of digoxin exist, including _dihydrodigoxin_ and _digoxigenin bisdigitoxoside_. Their glucuronidated and sulfated conjugates are thought to be produced through the process of hydrolysis, oxidation, and additionally, conjugation. The cytochrome P-450 system does not play a major role in digoxin metabolism, nor does this drug induce or inhibit the enzymes in this system.
In most patients, only small amounts of digoxin are metabolized, but the extent of metabolism is variable and may be substantial in some patients. Some metabolism presumably occurs in the liver, but digoxin is also apparently metabolized by bacteria within the lumen of the large intestine following oral administration and possibly after biliary elimination following parenteral administration. The extent of metabolism by bacteria in the large intestine following oral administration appears to vary inversely with the bioavailability of the preparation. Digoxin undergoes stepwise cleavage of the sugar moieties to form digoxigenin-bisdigitoxoside, digoxigenin-monodigitoxoside, and digoxigenin; these metabolites have progressively decreasing cardioactivity. Digoxigenin is subsequently epimerized and/or conjugated to form cardioinactive compounds. Digoxin also undergoes reduction of the lactone ring to form dihydrodigoxin, which also undergoes stepwise cleavage of the sugar moieties to form dihydrodigoxigenin-bisdigitoxoside, dihydrodigoxigenin-monodigitoxoside, and dihydrodigoxigenin; the reduced metabolites are essentially cardioinactive. Some patients may form substantial amounts of the reduced metabolites; data suggest that, in about 10% of patients receiving digoxin, about 40% or more of the drug excreted in urine will consist of reduced metabolites. Because of the rapid and enhanced absorption, use of liquid-filled capsules may minimize the formation of reduced metabolites in such patients. In patients who form substantial amounts of reduced metabolites, alteration of enteric bacterial flora by some anti-infective agents (e.g., erythromycin) may result in a substantial change in digitalization.
American Society of Health-System Pharmacists; Drug Information 2018. Bethesda, MD. 2018, p. 1821
Digoxin has a half-life of 1.5-2 days in healthy subjects. The half-life in patients who do not pass urine, usually due to renal failure, is prolonged to 3.5-5 days. Since most of the drug is distributed extravascularly, dialysis and exchange transfusion are not optimal methods for the removal of digoxin.
Eleven mothers given digoxin throughout pregnancy because of rheumatic heart disease were studied. Digoxin was identified in the placenta and, for the first time, in milk. ... The half-life of digoxin in the newborn was 36.2 +/- 5.43 hours (Mean +/- SEM); thus all the digoxin present at birth would be excreted within 10 to 11 days.
PMID:687540 Chan V et al; Br J Obstet Gynaecol 85 (8): 605-9 (1978)
Healthy volunteers received 0.4 mg IV/day for 14 days. Half-life 1.54 days. Distribution volume 807 L. Renal clearance 191 mL/min, indicating tubular secretion of digoxin. 1.8 fold accumulation once a day.
PMID:598412 Keller et al; Eur J Clin Pharmacol 12 (5): 387-92 (1977)
Values reported for the elimination half life of digoxin in dogs and cats have been highly variable, with vales reported from 14.4-56 hours for dogs; 30-173 hours for cats. Approximate elimination half-lives reported in other special include: sheep 7 hours; horses 17-29 hours; cattle 8 hours.
Plumb D.C. Veterinary Drug Handbook. 8th ed. (pocket). Ames, IA: Wiley-Blackwell, 2015., p. 440
The initial (distribution) half-life of digoxin is about 30 minutes after IV administration in both anephric patients and patients with normal renal function. In patients with normal renal function, digoxin has an elimination half-life of 34-44 hours. The elimination half-life of digoxin is prolonged in patients with renal failure; in anephric patients the elimination half-life is about 4.5 days or longer. The elimination half-life is decreased in patients with acute digoxin overdosage. Elimination half-life of digoxin is prolonged in hypothyroid patients and decreased in hyperthyroid patients. In patients with biliary fistulas, plasma half-life is unchanged. In undigitalized patients, institution of fixed daily digoxin maintenance therapy without an initial loading dose results in steady-state plasma concentrations after 4-5 elimination half-life (about 7 days in patients with normal renal function).
American Society of Health-System Pharmacists; Drug Information 2018. Bethesda, MD. 2018, p. 1821
Median serum half-life 35 hr in mature newborns and 57 hr in premature newborns.
PMID:865943 Lang et al; Pediatrics 59 (6): 902-6 (1977)
Digoxin exerts hemodynamic, electrophysiologic, and neurohormonal effects on the cardiovascular system. It reversibly inhibits the Na-K ATPase enzyme, leading to various beneficial effects. The Na-K ATPase enzyme functions to maintain the intracellular environment by regulating the entry and exit of sodium, potassium, and calcium (indirectly). Na-K ATPase is also known as the _sodium pump_. The inhibition of the sodium pump by digoxin increases intracellular sodium and increases the calcium level in the myocardial cells, causing an increased contractile force of the heart. This improves the left ventricular ejection fraction (EF), an important measure of cardiac function. Digoxin also stimulates the parasympathetic nervous system via the vagus nerve leading to sinoatrial (SA) and atrioventricular (AV) node effects, decreasing the heart rate. Part of the pathophysiology of heart failure includes neurohormonal activation, leading to an increase in norepinephrine. Digoxin helps to decrease norepinephrine levels through activation of the parasympathetic nervous system.
Cardiac glycosides have been used in the treatment of arrhythmias for more than 200 years. Two-pore-domain (K2P) potassium channels regulate cardiac action potential repolarization. Recently, K2P3.1 [tandem of P domains in a weak inward rectifying K+ channel (TWIK)-related acid-sensitive K+ channel (TASK)-1] has been implicated in atrial fibrillation pathophysiology and was suggested as an atrial-selective antiarrhythmic drug target. We hypothesized that blockade of cardiac K2P channels contributes to the mechanism of action of digitoxin and digoxin. All functional human K2P channels were screened for interactions with cardiac glycosides. Human K2P channel subunits were expressed in Xenopus laevis oocytes, and voltage clamp electrophysiology was used to record K+ currents. Digitoxin significantly inhibited K2P3.1 and K2P16.1 channels. By contrast, digoxin displayed isolated inhibitory effects on K2P3.1. K2P3.1 outward currents were reduced by 80% (digitoxin, 1 Hz) and 78% (digoxin, 1 Hz). Digitoxin inhibited K2P3.1 currents with an IC50 value of 7.4 uM. Outward rectification properties of the channel were not affected. Mutagenesis studies revealed that amino acid residues located at the cytoplasmic site of the K2P3.1 channel pore form parts of a molecular binding site for cardiac glycosides. In conclusion, cardiac glycosides target human K2P channels. The antiarrhythmic significance of repolarizing atrial K2P3.1 current block by digoxin and digitoxin requires validation in translational and clinical studies.
PMID:29643254 Schmidt C et al; J Pharmacol Exp Ther 365 (3): 614-623 (2018)
Low concentrations of cardiac glycosides including ouabain, digoxin, and digitoxin block cancer cell growth without affecting Na+,K+-ATPase activity, but the mechanism underlying this anti-cancer effect is not fully understood. Volume-regulated anion channel (VRAC) plays an important role in cell death signaling pathway in addition to its fundamental role in the cell volume maintenance. Here, we report cardiac glycosides-induced signaling pathway mediated by the crosstalk between Na+,K+-ATPase and VRAC in human cancer cells. Submicromolar concentrations of ouabain enhanced VRAC currents concomitantly with a deceleration of cancer cell proliferation. The effects of ouabain were abrogated by a specific inhibitor of VRAC (DCPIB) and knockdown of an essential component of VRAC (LRRC8A), and they were also attenuated by the disruption of membrane microdomains or the inhibition of NADPH oxidase. Digoxin and digitoxin also showed anti-proliferative effects in cancer cells at their therapeutic concentration ranges, and these effects were blocked by DCPIB. In membrane microdomains of cancer cells, LRRC8A was found to be co-immunoprecipitated with Na+,K+-ATPase a1-isoform. These ouabain-induced effects were not observed in non-cancer cells. Therefore, cardiac glycosides were considered to interact with Na+,K+-ATPase to stimulate the production of reactive oxygen species, and they also apparently activated VRAC within membrane microdomains, thus producing anti-proliferative effects.
PMID:30251696 Fujii T et al; Biochim Biophys Acta Mol Basis Dis 1864 (11): 3792-3804 (2018)
Cardiac glycosides inhibit the activity of sodium-potassium-activated adenosine triphosphatase (Na+-K+-ATPase), an enzyme required for active transport of sodium across myocardial cell membranes. Inhibition of this enzyme in cardiac cells results in an increase in the contractile state of the heart and it was believed that benefits of cardiac glycosides in heart failure were mainly associated with inotropic action. However, it has been suggested that benefits of cardiac glycosides may be in part related to enzyme inhibition in noncardiac tissues. Inhibition of Na+-K+-ATPase in vagal afferents acts to sensitize cardiac baroreceptors which may in turn decrease sympathetic outflow from the CNS. In addition, by inhibiting Na+-K+-ATPase in the kidney, cardiac glycosides decrease the renal tubular reabsorption of sodium; the resulting increase in the delivery of sodium to the distal tubules leads to the suppression of renin secretion from the kidneys. These observations led to the hypothesis that cardiac glycosides act in heart failure principally by attenuating the activation of the neurohormonal system, rather than by a positive inotropic action. Toxic doses of cardiac glycosides cause efflux of potassium from the myocardium and concurrent influx of sodium. Toxicity results in part from loss of intracellular potassium associated with inhibition of Na+-K+-ATPase. With therapeutic doses, augmentation of calcium influx to the contractile proteins with resultant enhancement of excitation-contraction coupling is involved in the positive inotropic action of cardiac glycosides; the role of Na+-K+-ATPase in this effect is controversial. /Cardiac glycosides/
American Society of Health-System Pharmacists; Drug Information 2018. Bethesda, MD. 2018, p. 1818








